Key takeaways
Ozempic (semaglutide) is a GLP-1 medication for type 2 diabetes. It may also be prescribed off-label for weight loss in people with obesity or overweight.
Research on semaglutide shows it can help people lose up to 15% of their body weight.
Ozempic may promote weight loss by decreasing appetite and helping you feel fuller after you eat.
Ozempic is not a “quick fix” weight loss solution. It’s a long-term medication meant to be used with a balanced diet and regular exercise for sustainable results.
Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Key takeaways
Ozempic (semaglutide) is a GLP-1 medication for type 2 diabetes. It may also be prescribed off-label for weight loss in people with obesity or overweight.
Research on semaglutide shows it can help people lose up to 15% of their body weight.
Ozempic may promote weight loss by decreasing appetite and helping you feel fuller after you eat.
Ozempic is not a “quick fix” weight loss solution. It’s a long-term medication meant to be used with a balanced diet and regular exercise for sustainable results.
By now you’ve likely heard of Ozempic. In 2021, the medication went viral across social media platforms and became a sensation among celebrities and influencers for its rapid impact on weight loss.
But you might not know that Ozempic isn’t technically a weight loss drug. The U.S. Food and Drug Administration (FDA) approved Ozempic for type 2 diabetes in 2017. Still, researchers soon discovered that some mechanisms of action that make semaglutide (the active ingredient in Ozempic) effective for blood sugar control also showed serious potential for weight loss.
Because of this and other possible health benefits, healthcare providers may prescribe Ozempic off-label for people with obesity or overweight.
With all of the hype around Ozempic, you might be wondering whether it’s effective or safe, or if it’s the right choice for you. Read on to learn everything you need to know about Ozempic for weight loss — how it works, side effects, cost, and more.
What is Ozempic?
Ozempic (semaglutide) is a prescription medication that’s FDA-approved to:
Treat type 2 diabetes
Reduce the risk of major cardiovascular health problems, such as heart attack, stroke, and cardiovascular death in adults with type 2 diabetes and heart disease
It’s in a class of medications called glucagon-like peptide-1 receptor agonists, or GLP-1s.
Ozempic comes in a pre-filled pen that you inject under the skin (in the thigh, abdomen, or upper arm) once each week. It’s available in four dose strengths: 0.25 mg, 0.5 mg, 1 mg, and 2 mg.
Semaglutide is also available under the brand name Wegovy.
Wegovy is FDA-approved for:
Weight management in people with obesity or those who have overweight and a weight-related comorbidity like high blood pressure, type 2 diabetes, and dyslipidemia (unhealthy levels of cholesterol and fat in the blood)
Reducing the risk of cardiovascular events in those with heart disease and obesity or overweight
While the two medications share the same active ingredient, Wegovy is available at a higher maximum dose strength than Ozempic.
What is Ozempic used for?
Ozempic is approved to help regulate blood sugar levels and reduce cardiovascular health risks in adults with type 2 diabetes.
Healthcare providers may also prescribe Ozempic off-label (when a drug is used for a condition other than its approved indication) to treat obesity or overweight. Providers typically use body mass index (BMI) as a metric for determining who might be a good candidate.
Find out how much you could lose
Provide your biometric data to get started.

0.0
Your BMI
Underweight
< 18.5
Healthy weight
18.5 - 24.9
Overweight
24.9 - 29.9
Obesity
> 30
How much does Ozempic cost?
The current list price without insurance is $997.58. Manufacturer savings programs and coupons may help reduce the monthly cost.
Insurance may also help mitigate costs, but coverage will vary by plan. Additionally, your insurance provider may not cover off-label use of Ozempic for weight loss.

How does Ozempic work?
GLP-1 medications like Ozempic work by mimicking the GLP-1 incretin hormone that the body produces naturally. The intestines release this hormone when we eat.
GLP-1 has several functions in the body, including increasing insulin secretion, reducing appetite, and slowing down parts of digestion. Ozempic works by binding to and activating these GLP-1 receptors in the body, which can help regulate blood sugar and may also promote weight loss.
Let’s take a closer look at each of these functions and how they may help with weight management.
Increasing satiety
Ozempic can help slow gastric emptying, which is the rate at which food moves from the stomach to the small intestine. This may make you feel full earlier and help you feel satisfied for longer after eating.
Decreasing hunger cues in the brain
One important role of the gut-brain axis—or, how our brains and gut communicate — is to tell our brains when we’re hungry or full.
GLP-1 medications like Ozempic activate the GLP-1 receptors in the brain, which can help suppress appetite and calm “food noise,” a nonmedical term that describes a type of intrusive preoccupation with food.
Improving insulin sensitivity
People with type 2 diabetes or obesity may also have insulin resistance, which occurs when cells stop responding as well to the hormone insulin.
Insulin helps move glucose (sugar) into cells to be used for energy. Insulin resistance can cause blood sugar levels to remain high and excess sugar to be stored in the body as fat.
The GLP-1 hormone that Ozempic and other weight loss injections mimic helps your pancreas produce more insulin. The increased insulin production can help lower elevated blood sugar levels and reduce insulin resistance. Enhancing insulin sensitivity may help promote weight loss.
Ozempic and weight loss: is it effective?
Yes. Research on semaglutide shows that, when combined with diet and exercise modifications, it may help people lose up to 15% of their body weight.
“The combined effect [of semaglutide] addresses both the physiological and behavioral aspects of weight management, making it a highly effective tool for significant and sustained weight loss,” says Sahar Takkouche, MD, the director of the Vanderbilt Weight Loss Center in Nashville, Tennessee.
Ozempic is not indicated for weight management, so little research exists on its effectiveness solely for weight loss. For example, most clinical trials reporting weight loss outcomes involved participants taking 2.4 mg of semaglutide, which is the maximum dose for Wegovy. The maximum dose of Ozempic is 2 mg of semaglutide.
While individual results will vary, research on semaglutide for type 2 diabetes and Wegovy clinical trials may still offer clues on how effective semaglutide is for weight loss overall.
Semaglutide and weight loss: what the research says
In one clinical trial studying people with type 2 diabetes, participants taking 0.5 mg of semaglutide lost an average of 8 pounds, and those taking 1.0 mg lost an average of 10 pounds after 30 weeks (about 7 months).
In another trial, participants with obesity or overweight who combined a weekly injection of 2.4 mg of semaglutide with a reduced-calorie diet and regular exercise lost an average of 15% of their weight over 68 weeks (about 1.3 years)compared to the placebo group.
In an observational study, researchers looked at weight loss outcomes for people with type 2 diabetes and obesity or overweight who took tirzepatide (Mounjaro) or semaglutide. They found that those taking 0.5 mg of semaglutide lost an average of 8.3% of their body weight after 12 months of treatment.
Ozempic is not a magic weight loss solution, but it can be considered a tool, along with diet and exercise changes, to help change the course of obesity and improve overall health.
“Obesity is not simply a matter of willpower,” explains Dr. Takkouche. “It’s a chronic, multifactorial condition influenced by genetics, metabolism, environment, and behavior.”
Due to these complex underlying factors, Dr. Takkouche says that lifestyle changes alone may not lead to significant or sustained weight loss for some people. In those cases, medications like Ozempic and other GLP-1s may also be needed.
“These interventions not only help individuals achieve weight loss but also improve related health conditions, such as diabetes, hypertension, and sleep apnea, ultimately enhancing quality of life and longevity,” Dr. Takkouche adds.
Is Ozempic safe? Side effects and risks
“Semaglutide is generally safe when used as prescribed,” Dr. Takkouche says.
“Like any medication, it does have potential side effects, the most common being gastrointestinal (GI) issues … Long-term studies are ongoing, but the benefits of significant weight loss, such as reduced cardiovascular risk and improved metabolic health, often outweigh these risks for many patients,” says Dr. Takkouche.
Common side effects
The most commonly reported side effects of Ozempic may include:
Abdominal pain
Diarrhea
Nausea
Vomiting
Common GI side effects tend to be mild, and they may go away as your body adjusts to the medication.
Keep in close contact with your healthcare provider so they can help you address any discomfort or unpleasant effects you might experience.
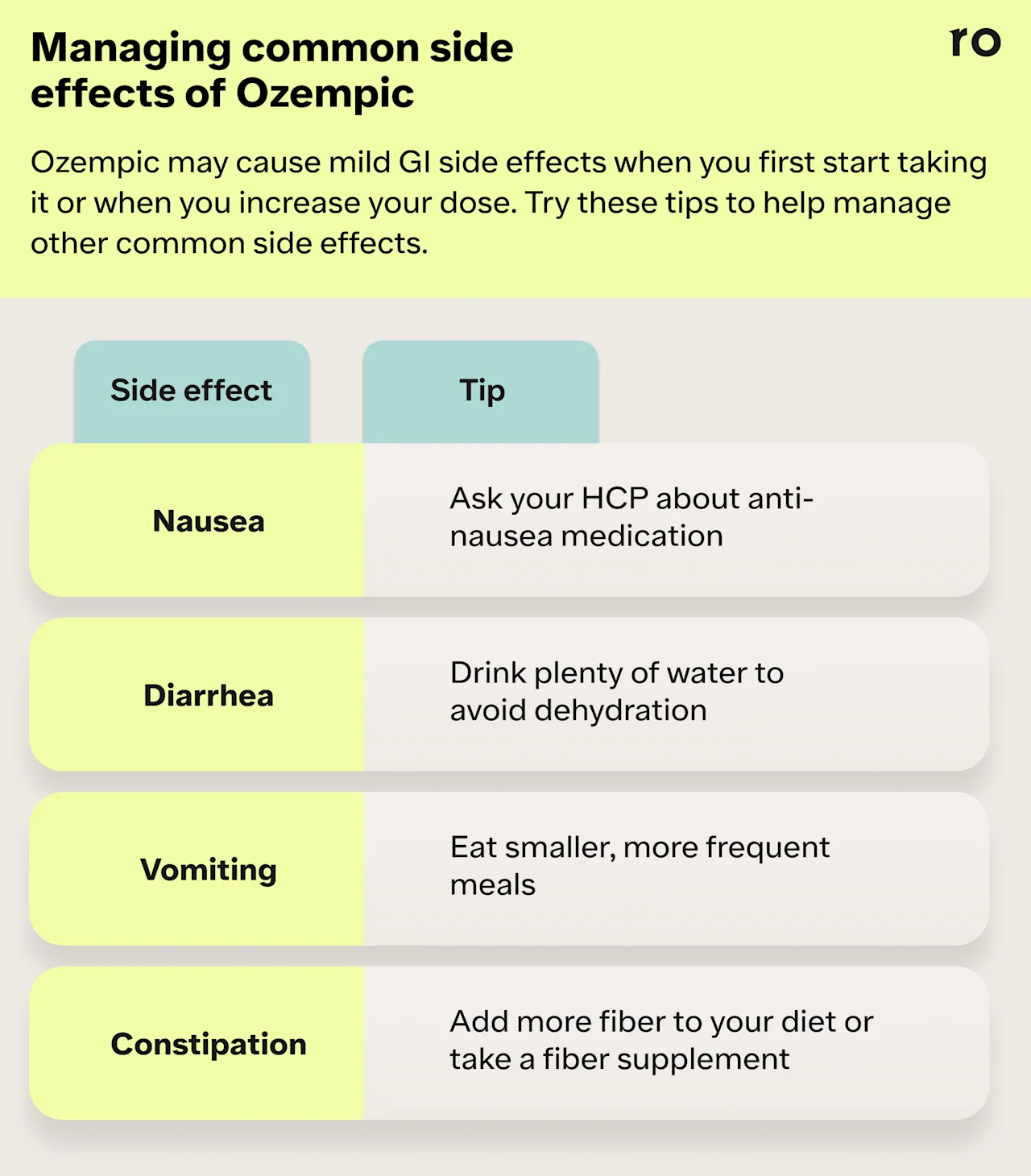
Tips for managing common side effects of Ozempic
The following strategies may help you manage or reduce common side effects:
Start at the lowest dose and slowly increase it over time. Common side effects tend to be most intense when a person first starts Ozempic or when they move up to the next dose strength. Starting at higher doses or jumping dose strengths can increase your risk for more severe side effects.
Stay hydrated. GI side effects like diarrhea can lead to dehydration, so make sure you’re drinking plenty of water each day.
Eat smaller, more frequent meals. This may help mitigate nausea and other GI discomfort as your body adjusts.
Ask your doctor about anti-nausea meds. Your provider may recommend a prescription or over-the-counter medication to help with nausea and vomiting.
Rare but serious adverse effects
Ozempic’s label contains a boxed warning for the potential risk of thyroid C-cell tumors, including medullary thyroid carcinoma. People who have a personal or family history of thyroid tumors are not good candidates for Ozempic or other GLP-1 medications. Your healthcare provider should screen you for risk factors before prescribing Ozempic or other GLP-1 medications.
Tell your doctor if you experience a lump or swelling in your neck, trouble swallowing, shortness of breath, or hoarseness, as these may be signs of a thyroid tumor.
“It’s crucial for patients to be under the care of a healthcare professional to monitor for any rare but serious side effects,” Dr. Takkouche says.
Though rare, Ozempic may increase your risk for more serious health complications. These may include:
Allergic reactions. Symptoms may include facial or throat swelling, difficulty breathing or swallowing, itching or rash, fainting or feeling dizzy, or rapid heartbeat.
Inflammation of the pancreas (pancreatitis). Symptoms may include severe abdominal pain that doesn’t go away and sometimes back pain.
Gallbladder problems (e.g. gallstones or gallbladder inflammation). Symptoms may include pain in the upper abdomen, fever, yellowing of the skin or eyes, or clay-colored stools.
Kidney problems (kidney failure). People with existing kidney problems may notice worsening symptoms if they become chronically dehydrated.
Low blood sugar (hypoglycemia). Symptoms may include dizziness or lightheadedness, blurred vision, mood changes, sweating, slurred speech, hunger, confusion, drowsiness, shakiness, weakness, headache, rapid heartbeat, or feeling jittery.
Vision changes. Symptoms may include blurred vision, floaters, or spots. For people with type 2 diabetes who also have a history of diabetic retinopathy (a condition that can cause blood vessel damage in the retina), Ozempic may worsen symptoms. People with a known history of diabetic retinopathy should be closely monitored while taking this medication.
Gastroparesis or bowel obstruction. Some research has found that semaglutide may be associated with gastroparesis (stomach paralysis) and bowel obstruction. Symptoms can include bloating, abdominal pain, and vomiting.
Pulmonary aspiration during general anesthesia. This has been reported in patients undergoing elective surgeries or procedures while taking GLP-1 medications.
Potential medication interactions
Ozempic may interact with other medications, including some blood pressure medications, diuretics, or drugs like insulin that can impact blood sugar levels.
Be sure to tell your doctor about all the prescription or over-the-counter medications or supplements you’re taking.
Who should not take Ozempic?
Ozempic may not be suitable for everyone. You should avoid taking Ozempic if:
You’re under 18
You’re allergic to any medication ingredients
You’re pregnant, breastfeeding, or about to become pregnant
You or a family member have ever had medullary thyroid carcinoma (a type of thyroid cancer) or multiple endocrine neoplasia type 2 (a condition that affects the endocrine system)
You have a personal or family history of kidney problems, pancreatitis, or diabetic retinopathy
Ozempic vs. Wegovy and other alternatives
Ozempic may not be the best option for everyone—side effects, health goals, cost, and your provider’s recommendations will all factor into finding the right medication for you.
Here’s a quick look at some alternatives to Ozempic for weight loss.
Wegovy
Wegovy is an injectable GLP-1 medication and another brand name for semaglutide. It’s FDA-approved for weight management in adults and children aged 12 and older with obesity and for people with overweight and certain weight-related health conditions like high blood pressure or high cholesterol. Wegovy may also help reduce cardiovascular risks like heart attack and stroke.
Because Wegovy and Ozempic share the same active ingredient, they essentially work in the same way. However, Wegovy is available in different dose strengths: 0.25 mg, 0.5 mg, 1 mg, 1.7 mg, and 2.4 mg. In clinical trials, participants taking 2.4 mg of semaglutide weekly lost an average of 15% of their body weight after 1.3 years.
The list price for Wegovy is $1,349.02 without discounts or rebates. However, insurance, coupons, and other savings programs may be able to help mitigate the cost.
No insurance? Or just prefer to pay with cash? Through Ro, you can get Wegovy for the following cash prices:
$199 per month for the first two months for a limited time (only valid for 0.25 mg and 0.5 mg doses)
$349 per month thereafter
The most common side effects of Wegovy are similar to those reported with Ozempic and include nausea, diarrhea, vomiting, abdominal pain, constipation, headache, fatigue, dizziness, and injection site reactions.
Zepbound (tirzepatide)
Zepbound is a dual GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptor agonist. It’s also a weekly injectable medication that’s indicated for weight management in adults with obesity and adults with overweight and other comorbid health conditions.
The active ingredient in Zepbound is tirzepatide, which is also available under the brand name Mounjaro to treat type 2 diabetes.
Zepbound comes in a pre-filled pen or a single-dose vial, and has six dose strengths: 2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, and a maximum dosage of 15 mg.
Zepbound works similarly to other GLP-1 medications, but the dual action of GLP-1 and GIP may enhance its effectiveness for weight loss.
In one phase 3 clinical trial, participants taking 5 mg of tirzepatide weekly lost an average of 15% of their body weight after 72 weeks. In that same trial, those taking the maximum dosage of tirzepatide (15 mg) lost roughly 20.9% of their body weight over the same period.
The list price for Zepbound is $1,086.37. Insurance, coupons, or savings programs — including Ro and Eli Lilly’s self-pay option — can help cover the cost of Zepbound each month.
The cost of Zepbound may also vary depending on whether you use the single-use pen or the single-dose vial. Through Ro’s cash-pay option, single-dose Zepbound vials are available for the following cash prices:
$299 per month: 2.5 mg dose
$399 per month: 5 mg dose
$449 per month (with manufacturer offer): 7.5 mg, 10 mg, 12.5 mg, 15 mg doses
Zepbound side effects are similar to other GLP-1 medications. The most common side effects include nausea, diarrhea, vomiting, constipation, abdominal pain, injection site reactions, hair loss, fatigue, and upset stomach.
Saxenda (liraglutide)
Saxenda is also an injectable GLP-1 medication for weight loss. Unlike other medications in this class, Saxenda is taken daily.
It’s approved for weight loss in adults with obesity or those who are overweight and have a weight-related comorbidity like high blood pressure, type 2 diabetes, and dyslipidemia (unhealthy levels of cholesterol and fat in the blood). It’s also approved for children aged 12 and up who have obesity.
Saxenda comes in five dose strengths: 0.6 mg, 1.2 mg, 1.8 mg, 2.4 mg, and 3 mg. Similar to other GLP-1 medications, Saxenda may promote weight loss by reducing hunger cues and helping you to feel fuller and more satisfied after eating.
Research shows that liraglutide (the active ingredient in Saxenda) can also be an effective tool for weight loss. In one 56-week double-blind trial, participants taking 3 mg of liraglutide lost between 5%–10% of their body weight.
The list price for Saxenda before insurance, coupons, or other discounts is $1,349.02 per month.
The most common Saxenda side effects include nausea, diarrhea, constipation, vomiting, injection site reactions, headache, low blood sugar, indigestion, fatigue, dizziness, upper abdominal pain, and bloating.
Oral weight loss medications
Some oral prescription and over-the-counter (OTC) medications may also be effective tools for weight loss. Some of the most common weight loss pills include:
Contrave (naltrexone/bupropion)
Qsymia (phentermine/topiramate)
Adipex-P (Phentermine)
Lomaira (Phentermine)
These pills are taken daily (in some cases, twice daily), and dosing will vary based on the medication. These medications may promote weight loss by suppressing appetite and increasing feelings of fullness after and in between meals. Some oral medications for weight loss also work by reducing the amount of fat your body absorbs from the food you eat.
One review of research on FDA-approved weight loss treatments found that oral medications can be effective for weight loss, though they may not produce as much weight loss as GLP-1s. According to that review of clinical trials for orlistat, phentermine, and naltrexone/bupropion, these medications helped people lose 5% or more of their weight when combined with lifestyle changes.
Common side effects of oral weight loss medications include GI symptoms like nausea, vomiting, or constipation. Other side effects, such as dizziness, headaches, or blurry vision, have also been reported with some weight loss medications.
The cost of oral medications varies by drug. For example, the retail price for a 30-day supply of Contravel ranges from about $99 with a savings card to more than $600, depending on the pharmacy or other savings programs or coupons.
How long do I have to take Ozempic?
Your healthcare provider will offer guidance on how long you’ll need to take Ozempic, which will depend on your health status, weight loss goals, and how well you tolerate the medication.
Generally, people take Ozempic for a long time — usually for a year or longer — to experience sustained weight loss results and blood sugar control.
Some research shows that stopping semaglutide too soon may lead to regaining the weight you lost while taking the medication.
For example, in one randomized controlled trial, after participants discontinued 2.4 mg of semaglutide and stopped lifestyle changes for a full year, they regained about two-thirds of the weight they had lost. This rebound weight gain occurred after participants had been on the medication for 1.3 years and made lifestyle changes, including diet and exercise, during that time.
Researchers are still trying to understand why weight regain may occur after stopping Ozempic or using other weight loss medications.
One theory involves the “set point.” Our bodies appear to have a set weight point or a predetermined weight the body tries to maintain, based on genetics, changes in gene expression, environmental factors, and more. This means that even when you lose weight, your body may do what it can to return to its predetermined weight.
Ozempic and other GLP-1 medications may temporarily suppress the mechanisms in the body that try to maintain a higher weight. When you stop the medication, however, your body may try to return to its set weight point.
Current research in humans does not show that GLP-1s can alter set weight points. However, healthy lifestyle habits around diet, fitness, and stress management may help to suppress the body’s set weight point to some extent.
How can I optimize weight loss with Ozempic?
“Patients should understand that semaglutide is most effective when combined with lifestyle changes, such as a healthy diet and regular physical activity, making it part of a comprehensive care plan,” Dr. Takkouche says.
You can make several sustainable lifestyle changes to complement Ozempic’s weight loss effects and improve overall health. These habits may also help mitigate rebound weight gain if you decide to stop taking Ozempic.
Lifestyle habits to support weight loss might include:
Reducing or eliminating ultra-processed foods. Foods like chips, processed meat, and soft drinks are high in sodium, unhealthy fats, and added sugar, which can contribute to insulin resistance and the accumulation of visceral fat.
Eating more fruits and vegetables. These high-fiber foods feed the microbiome, creating short-chain fatty acids, which help produce natural GLP-1. They are also loaded with antioxidants, which can help lower inflammation and improve overall health.
Including more protein in your diet. Protein can help you feel more satisfied and can help slow the absorption of glucose into the bloodstream, which can, in turn, help with insulin sensitivity. Protein also supports muscle, and more muscle can also make you more insulin-sensitive and increase how many calories you burn at rest.
Incorporating strength training into your workouts. Increasing muscle mass can boost the amount of calories you burn at rest and improve insulin sensitivity. Strength training is also particularly important for people on GLP-1 medications, such as Ozempic, since some of the weight you may lose may include some muscle.
Upping your cardio. Aerobic exercise can help get your heart rate up and improve your endurance. A good rule of thumb is to choose activities you enjoy—whether that’s swimming, running, rowing, playing pickleball, etc. The more you enjoy an activity, the more you’re likely to keep doing it.
Getting at least 7-9 hours of quality sleep per night. Poor sleep can make you more insulin-resistant the next day and may drive cravings. Sleep also helps regulate cortisol, the “stress hormone.” Although we need cortisol to function in our daily lives, too much of this hormone contributes to weight gain.
Finding creative ways to relieve stress. Reducing stress can be easier said than done in a world where we’re constantly bombarded with stressors big and small. However, chronic stress increases cortisol, which can lead to weight gain. Techniques such as meditation, journaling, or devoting time to your hobbies may be effective tools for managing stress.
How do I get Ozempic for weight loss?
Talk to your healthcare provider if you have questions about how to get Ozempic for weight loss. They can evaluate whether you meet the criteria for off-label use, and review your personal and family health history, weight loss goals, and other factors to determine if Ozempic is an appropriate and safe option for you.
In some cases, your provider may recommend an alternative medication, such as Wegovy or Zepbound.
Some private insurance companies may not cover the cost of off-label Ozempic or weight loss medications in general. Check with your plan to see what coverage options are available to you. If your medication isn’t covered, you may still be eligible for coupons or manufacturer discounts to help mitigate monthly costs.
You may also qualify for an online weight loss program, such as the Ro Body membership.
This comprehensive offering connects you with a licensed healthcare provider to review your health history and other factors to determine if you are a good candidate for GLP-1 treatment. Your provider can then provide a holistic and personalized treatment program, including medication, health coaching, resources, and ongoing weight loss support.
If your healthcare provider prescribes a GLP-1 medication, Ro’s concierge can also work with your insurance company to help get your prescription covered.
Rx weight loss with Ro
Get access to prescription weight loss medication online
Bottom line
Obesity is a chronic condition, and sometimes diet and exercise alone are not enough to promote weight loss. Medications or other interventions may be needed.
GLP-1 medications like Ozempic are not magic solutions, but can be effective tools for weight loss and may help people lose 10% or more of their body weight.
There are several alternatives to Ozempic for weight loss, including Wegovy, Zepbound, and Saxenda.
Weight loss medications are meant to be used with diet and exercise modifications to achieve optimal and sustainable results. Additionally, these medications are designed to be taken long-term (a year or longer).
Like many medications, Ozempic may cause side effects or pose other health risks for certain people. Your healthcare provider can help you determine if Ozempic is right for you.
Frequently asked questions (FAQs)
What happens if you take Ozempic without diabetes?
The risks of taking Ozempic without diabetes are similar to those in people with diabetes and may include common GI side effects, potential medication interactions, and rare but serious health complications like pancreatitis or thyroid tumors.
That said, Ozempic is indicated for type 2 diabetes and is not intended as a weight loss drug. If you’re curious about medications specifically designed for weight loss, your healthcare provider may recommend alternatives such as Wegovy, Zepbound, or Saxenda.
How much weight can you lose on Ozempic in a month?
How much weight you can lose in a month on Ozempic will depend on individualized factors such as your dosage, starting weight, underlying health conditions, and more.
Who cannot take Ozempic?
Do not use Ozempic if you:
Are under 18
Are allergic to any medication ingredients
Are pregnant, breastfeeding, or about to become pregnant
Have a personal or family history of medullary thyroid carcinoma (a type of thyroid cancer) or multiple endocrine neoplasia type 2
Additionally, if you have a personal or family history of kidney problems, pancreatitis, or diabetic retinopathy, talk to your doctor about these issues. Ozempic may not be suitable for you.
What is the downside of Ozempic?
As with any medication, Ozempic can cause mild side effects, such as nausea and vomiting, and may also present rare but serious side effects and health complications. The medication needs to be taken long-term for better blood sugar control or to produce and, in some cases, maintain weight loss results. Ozempic can also be expensive, especially if not covered by your insurance.
Does Ozempic help you lose belly fat?
Ozempic may help you lose belly fat by encouraging weight loss overall. However, research shows that GLP-1 medications like Ozempic also significantly reduce visceral fat, a type of fat that surrounds internal organs and can cause chronic health issues. This type of fat is often called abdominal or belly fat because it pushes the belly outward.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Ozempic Important Safety Information: Read more about serious warnings and safety info.
Wegovy Important Safety Information: Read more about serious warnings and safety info.
GLP-1 Important Safety Information: Read more about serious warnings and safety info.
Mounjaro Important Safety Information: Read more about serious warnings and safety info.
Zepbound Important Safety Information: Read more about serious warnings and safety info.
Saxenda Important Safety Information: Read more about serious warnings and safety info.
References
Baggio, L. L. & Drucker, D. J. (2014). Glucagon-like peptide-1 receptors in the brain: controlling food intake and body weight. The Journal of Clinical Investigation, 124(10), 4223. doi: 10.1172/JCI78371. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4191040/
Calanna, S., Christensen, M., Holst, J. J., et al. (2013). Secretion of glucagon-like peptide-1 in patients with type 2 diabetes mellitus: systematic review and meta-analyses of clinical studies. Diabetologia, 56(5), 965. doi: 10.1007/s00125-013-2841-0. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3687347
Collins, L. & Costello, R. A. (2024). Glucagon-Like Peptide-1 Receptor Agonists. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK551568/
GoodRx. (n.d.). Contrave. Retrieved from https://www.goodrx.com/contrave
Hayashi, D., Edwards, C., Emond, J. A., et al. (2023). What is food noise? A conceptual model of food cue reactivity. Nutrients, 15(22), 4809. doi: 10.3390/nu15224809. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10674813/
Ida, S., Kaneko, R., Imataka, K., et al. (2021). Effects of antidiabetic drugs on muscle mass in type 2 diabetes mellitus. Current Diabetes Reviews, 17(3), 293-303. doi: 10.2174/1573399816666200705210006. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32628589/
Idrees, Z., Cancarevic, I., & Huang, L. (2022). FDA-Approved Pharmacotherapy for Weight Loss Over the Last Decade. Cureus, 14(9), e29262. doi: 10.7759/cureus.29262. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9579826/
Jastreboff, A. M., Aronne, L. J., Ahmad, N. N., et al. (2022). Tirzepatide Once Weekly for the Treatment of Obesity. The New England Journal of Medicine, 387(3), 205–216. doi: 10.1056/NEJMoa2206038. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa2206038
Jensterle, M., Ferjan, S., Ležaič, L., et al. (2023). Semaglutide delays 4-hour gastric emptying in women with polycystic ovary syndrome and obesity. Diabetes, Obesity, and Metabolism, 25(4), 975-984. doi: 10.1111/dom.14944. Retrieved from https://pubmed.ncbi.nlm.nih.gov/36511825/
Knudsen, L. B. & Lau, J. (2019). The discovery and development of liraglutide and semaglutide. Frontiers in Endocrinology (Lausanne), 10, 155. doi: 10.3389/fendo.2019.00155. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31031702/
Kommu, S. & Whitfield, P. (2024). Semaglutide. StatPearls. Retrieved on Nov. 12, 2024 from https://www.ncbi.nlm.nih.gov/books/NBK603723/
Lilly. (n.d.). How much should I expect to pay for Zepbound (tirzepatide)? Retrieved from https://pricinginfo.lilly.com/zepbound
Liu, J., Yang, X., Yu, S., & Zheng, R. (2018). The leptin resistance. Advances In Experimental Medicine And Biology, 1090, 145-163. doi: 10.1007/978-981-13-1286-1_8. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30390289/
Montecinos, K., Kania, B., & Goldberg, D. J. (2024). Semaglutide “Ozempic” Face and Implications in Cosmetic Dermatology. Dermatological Reviews, 5(5). https://onlinelibrary.wiley.com/doi/epdf/10.1002/der2.70003
Müller, T. D., Finan, B., Bloom, S. R., et al. (2019). Glucagon-like peptide 1 (GLP-1). Molecular Metabolism, 30, 72-130. doi: 10.1016/j.molmet.2019.09.010. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31767182/
Novo Nordisk-a. (2023). Find out the cost for Ozempic. Retrieved from https://www.novocare.com/diabetes/products/ozempic/explaining-list-price.html
Novo Nordisk. (2017). Ozempic® (semaglutide) approved in the US. Retrieved from https://www.novonordisk.com/content/nncorp/global/en/news-and-media/news-and-ir-materials/news-details.html?id=712
Novo Nordisk-b. (2023). What is the list price for Saxenda and will it impact me? Retrieved from https://www.novocare.com/obesity/products/saxenda/explaining-list-price.html
Novo Nordisk. (2024). What is the list price for Wegovy and will it impact me? Retrieved from https://www.novocare.com/obesity/products/wegovy/let-us-help/explaining-list-price.html
Pi-Sunyer, X., Astrup, A., Fujioka, K., et al. (2015). A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management. The New England Journal Of Medicine, 373(1), 11–22. doi: 10.1056/NEJMoa1411892. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa1411892
Popoviciu, M. S., Păduraru, L., Yahya, G., et al. (2023). Emerging role of glp-1 agonists in obesity: a comprehensive review of randomised controlled trials. International Journal of Molecular Sciences, 24(13), 10449. doi: 10.3390/ijms241310449. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10341852/
Rodriguez, P. J., Goodwin Cartwright, B. M., Gratzl, S., et al. (2024). Semaglutide vs Tirzepatide for Weight Loss in Adults With Overweight or Obesity. JAMA Internal Medicine, 184(9), 1056–1064. doi: 10.1001/jamainternmed.2024.2525. Retrieved from https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2821080
Ryan, D. H., Lingvay, I., Deanfield, J., et al. (2024). Long-term weight loss effects of semaglutide in obesity without diabetes in the SELECT trial. Nature Medicine, 30(7), 2049-2057. doi: 10.1038/s41591-024-02996-7. Retrieved from https://www.nature.com/articles/s41591-024-02996-7
Sodhi, M., Rezaeianzadeh, R., Kezouh, A., et al. (2023). Risk of gastrointestinal adverse events associated with glucagon-like peptide-1 receptor agonists for weight loss. JAMA, 330(18), 1795. doi: 10.1001/jama.2023.19574. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10557026/
U.S. Food & Drug Administration (FDA). (2025). Highlights of Prescribing Information: Wegovy (semaglutide) injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/215256s015lbl.pdf
U.S. Food and Drug Administration (FDA). (2018). Understanding unapproved use of approved drugs “off label”. Retrieved from https://www.fda.gov/patients/learn-about-expanded-access-and-other-treatment-options/understanding-unapproved-use-approved-drugs-label
Wadden, T. A., Chao, A. M., Moore, M., et al. (2023). The role of lifestyle modification with second-generation anti-obesity medications: comparisons, questions, and clinical opportunities. Current Obesity Reports, 12(4), 453. doi: 10.1007/s13679-023-00534-z. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10748770/
Wilding, J. P. H., Batterham, R. L., Calanna, S., et al. (2021). Once-weekly semaglutide in adults with overweight or obesity. New England Journal of Medicine, 384(11), 989-1002. doi: 10.1056/NEJMoa2032183. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa2032183