Key takeaways
Headaches can be a side effect of semaglutide. They’re considered a common side effect of Wegovy, but not Ozempic or Rybelsus.
Dehydration and low blood sugar are the most likely causes of semaglutide headaches, so staying hydrated and eating well is important.
Headaches may improve on their own, but if they don’t, adjusting your dosage, tracking your triggers, or changing your treatment plan may be a smart next step.
Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Key takeaways
Headaches can be a side effect of semaglutide. They’re considered a common side effect of Wegovy, but not Ozempic or Rybelsus.
Dehydration and low blood sugar are the most likely causes of semaglutide headaches, so staying hydrated and eating well is important.
Headaches may improve on their own, but if they don’t, adjusting your dosage, tracking your triggers, or changing your treatment plan may be a smart next step.
Semaglutide, the active ingredient in the drugs Ozempic, Wegovy, and Rybelsus, is well known for its ability to cause weight loss, control blood sugar, and reduce cardiovascular risk. Many people who’ve taken the medication also talk about side effects like nausea and constipation. But what about semaglutide headaches?
Does semaglutide cause headaches, or could something else be going on? Whether you’re already experiencing headaches while taking semaglutide — or worried that you will once you start taking the drug — read on. We explain possible causes of semaglutide headaches, and what you can do to prevent and treat them.
Does semaglutide cause headaches?
While some people may experience headaches while taking semaglutide, not necessarily everyone will. Semaglutide headaches appear to be more common when someone is taking a higher dose of the medication, such as Wegovy 2.4 mg.
In fact, headache is listed as one of the most common Wegovy side effects.
In a clinical trial of adults taking Wegovy 2.4 mg for weight management,
14% of adults experienced headaches
17% of pediatric patients ages 12 and older experienced headaches
This is compared to only 10% of adults and 16% of pediatric patients who were taking a placebo.
In another clinical trial, just over 15% of Wegovy users experienced headaches, compared to just over 12% among those taking a placebo.
In these studies, all participants followed a reduced-calorie diet and increased exercise.
Note that headaches were also quite common in the placebo groups, with at least 10% of participants experiencing them despite not taking the active medication. This suggests that adjusting to lifestyle changes — which can affect hydration, blood sugar, and energy levels — may also contribute to headaches while you’re trying to lose weight.
Headache is not listed as a common side effect of Ozempic or Rybelsus, but that doesn’t mean you won’t experience a headache if you’re taking one of these drugs.
A review of several clinical studies found that people taking Ozempic weren’t any more likely to experience headaches than those taking a placebo. However, it’s worth mentioning that this study was funded by Novo Nordisk, the makers of Ozempic.
How long does a semaglutide headache last?
How long a semaglutide headache lasts can depend on what’s causing it, says Paul Rosenberg, MD, head plastic surgeon at the New Jersey Breast Reduction Center, where he often treats patients for weight loss with semaglutide prior to performing surgery.
“If headaches are related to dehydration or low blood sugar, addressing the root cause is often the best way to provide fast relief,” Dr. Rosenberg explains. “If the headaches are part of the body adjusting to the medication, they may persist intermittently for the first couple weeks, particularly after dose increases.”
In general, though, “most headaches are temporary and tend to resolve within a few hours to a couple of days,” he adds.
Why can semaglutide cause headaches?
When semaglutide causes headaches, dehydration and low blood sugar are likely culprits. It can also be coincidental: you’re experiencing headaches, but it’s not actually caused by the medicine itself. Let’s take a closer look at these potential causes of semaglutide headaches.
1. Dehydration
“Headaches are a second-order side effect of semaglutide that can occur when the patient gets dehydrated,” Dr. Rosenberg says. “Patients tend to get dehydrated on semaglutide due to slowed digestion, reduced thirst cues, and potential nausea or vomiting. For many patients drinking more water can often make a big difference.”
Dehydration can happen if you’re simply not drinking enough water to stay hydrated. If you’re experiencing other common adverse effects of semaglutide—like nausea, vomiting, or diarrhea (or all of the above) — you could be losing even more fluids than your body needs, leading to dehydration.
And if you’re already prone to migraines, being dehydrated can make them more likely to happen.
Lack of hydration can also cause or worsen kidney problems. Acute kidney injury can be a rare side effect of semaglutide. It can coincide with dehydration and the gastrointestinal side effects (e.g. diarrhea, nausea, vomiting) that can occur when taking semaglutide.
If you have kidney issues, talk to your healthcare provider if you experience these side effects on semaglutide.
2. Low blood sugar
A headache can be a symptom of low blood sugar, which can be more likely when taking glucose-lowering medications like semaglutide — especially if you are taking semaglutide in combination with insulin or sulfonylureas (which also lowers blood sugar). Low blood sugar has also been known to trigger or worsen migraines in some people.
Prior to starting semaglutide, be sure to share a full list of all medications you are taking with your healthcare provider. If you are taking insulin, sulfonylureas, or other diabetes medications that lower blood sugar, your healthcare provider may lower the dosage of these other medications to reduce your risk of experiencing hypoglycemia (low blood sugar).
They should also talk to you about how to recognize the signs of low blood sugar, and recommend keeping a source of sugar (like juice or glucose tablets) on hand in case it happens.
Besides headache, other signs and symptoms of low blood sugar include:
Blurry vision
Rapid heartbeat
Irritability or mood changes
Hunger
Shaking or trembling
Sweating
Skin tingling or numbness
Tiredness
Difficulty thinking clearly
3. Coincidence
When it comes to what causes semaglutide headaches, the answer may be as simple as plain old coincidence.
Headaches are quite common. On any given day, nearly 16% of people experience a headache. And roughly half of people worldwide have a headache disorder, including migraine and tension-type headache. Women and people ages 25–40 are more likely to experience headaches.
Common causes of headaches include:
Hangover
TMJ syndrome (pain and inflammation in your jaw)
Depression
Anxiety
Physical strain or injury to the head or neck
Caffeine withdrawal
Lack of sleep
Swelling in the sinuses
Another health condition, such as a cold, flu, fever, or premenstrual syndrome (PMS)
Migraines can be triggered by sound, light, or certain foods such as chocolate, cheese, or monosodium glutamate (MSG).
Headaches can also be a warning sign of something more serious, such as a brain infection or carbon monoxide poisoning. If your headaches persist, contact a healthcare professional.
How to prevent and treat a semaglutide headache
Headaches are no fun, no matter what’s causing them. Here are seven ways to prevent and/or treat semaglutide headaches.
1. Stay hydrated
To prevent semaglutide headaches, Dr. Rosenberg recommends you “stay well hydrated throughout the day, even if [you] don’t actually feel thirsty.”
A study of people with migraines found that those who drink more water experienced fewer and less intense headaches.
Drinking plenty of fluids may not only help prevent dehydration and semaglutide headaches, but also ease some of semaglutide’s other side effects, such as nausea. Remember: You can also increase your water intake by eating water-rich foods, such as soup, yogurt, and gelatin.
2. Eat a blood-sugar-friendly diet
It’s important to keep your blood sugar levels in check when taking semaglutide, not only because you may be taking semaglutide to manage type 2 diabetes, but also given the link between low blood sugar and headache.
There’s also evidence that a low-glycemic diet can help treat migraine.
“Eating balanced meals with enough protein and complex carbs can help prevent blood sugar crashes that may trigger headaches,” Dr. Rosenberg says.
For help putting together a meal plan that supports healthy blood sugar levels while ensuring proper nutrition, you may want to talk to a registered dietitian (RD) or nutritionist while taking semaglutide.
3. Learn your migraine triggers
People who experience migraines often have specific triggers that are unique to them, such as bright lights, loud noise, intense heat, or too much caffeine or alcohol.
Keeping a diary can help you identify your triggers. Note what you ate or experienced before the migraine came on, and see if you notice any commonalities. Once you know your triggers, you can take steps to avoid them.
4. Talk to your healthcare provider about your dosing schedule
The recommended dosing schedule for semaglutide follows a titration process. Typically, you start at a low dosage of the medication and gradually increase your dosage over a period of weeks to months until you find an effective maintenance dosage for you.
“Gradually increasing the dosage of the medication rather than jumping to a higher dose too quickly can allow the body more time to adjust and prevent headaches from occurring,” Dr. Rosenberg explains.
Your healthcare provider should guide you through this dosing process. But it’s important to keep them informed of any side effects you are experiencing, headaches included. If needed, they can slow down your semaglutide dosing schedule to help keep side effects more manageable.
5. Consider over-the-counter (OTC) medication
“If headaches persist, OTC pain relievers like acetaminophen or ibuprofen can provide relief,” Dr. Rosenberg says. “But always check with your healthcare provider before mixing or taking any new medications.”
If OTC pain relievers aren’t helping, talk to your healthcare provider. They can help identify the cause of your headaches and, if appropriate, discuss prescription medications for headache. It’s a good idea to share a list of all the medications you are taking to avoid any potential side effects or drug interactions.
6. Wait it out
You can take steps to prevent semaglutide headaches, such as staying hydrated, avoiding triggers, and following a healthy diet. But you may still experience headaches. In that case, you may just need to give it time, especially if you’ve only recently started taking semaglutide.
“Headaches tend to become less frequent for most patients over time as the body adjusts to the medication,” Dr. Rosenberg says. “The first couple weeks and after dose increases are the most common times for headaches to persist.”
If your headaches are severe or persistent, talk to your healthcare provider to make sure they’re not a sign of something more serious that requires medical attention.
7. Consider semaglutide alternatives
If your semaglutide headaches or other side effects become too much, talk to your healthcare provider about whether an alternative treatment could be a better fit for you.
There are several glucagon-like peptide-1 (GLP-1) medications besides semaglutide, including:
Liraglutide (Saxenda, Victoza)
Dulaglutide (Trulicity)
There are also other medications that treat obesity, type 2 diabetes, and cardiovascular disease. Some of these medications may have a more favorable side effect profile for you or be less likely to cause headaches.
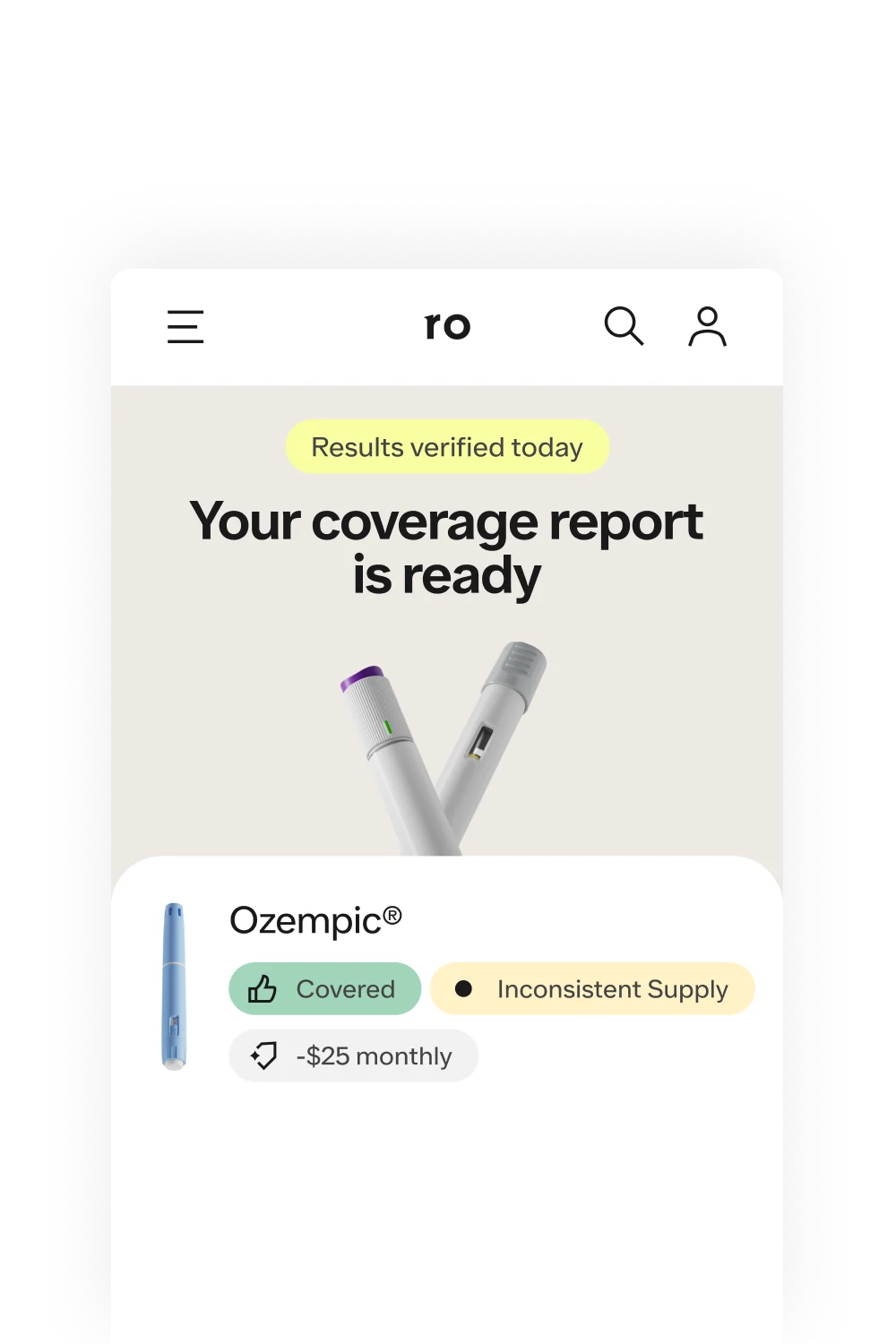
For example, headaches are not a known side effect of Zepbound. And some may even be cheaper than semaglutide or covered by your insurance. Talk to your healthcare provider about your options.
Rx weight loss with Ro
Get access to prescription weight loss medication online
Bottom line
Semaglutide headaches can be frustrating, but in many cases, they are preventable and treatable. Whether they stem from dehydration, low blood sugar, or other factors, understanding the possible causes can help you take proactive steps to reduce their frequency and severity.
Semaglutide can cause headaches, but not for everyone. Headaches are more commonly reported with higher doses of semaglutide, such as those typical of Wegovy, though they may also occur with Ozempic or Rybelsus.
Dehydration and low blood sugar are the most likely culprits. Semaglutide lowers blood sugar and has side effects like nausea and vomiting, which can lead to hypoglycemia or dehydration—both of which can trigger headaches.
Tracking your triggers can help. Keeping a diary of what was going on before each headache can help identify specific triggers and patterns.
Staying hydrated and eating well may prevent semaglutide headaches. By drinking lots of fluids and following a healthy diet that emphasizes low-glycemic foods, you may be able to minimize pain and discomfort while you continue on your weight loss journey.
Other treatment options are available. Over-the-counter pain relievers and prescription medication can help if headaches persist. You may also want to explore other alternatives to Wegovy or Ozempic with your healthcare provider.
If your headaches are severe, long-lasting, or accompanied by other concerning symptoms, it’s important to reach out to your healthcare provider to ensure they aren’t a sign of a more serious issue.
Frequently asked questions (FAQs)
Does Wegovy cause headaches?
Yes, Wegovy can cause headaches. Not only that, but headaches are listed as one of the drug’s most common side effects. In clinical trials of Wegovy 2.4 mg, 14% of adults and 17% of pediatric patients ages 12 and older experienced headaches. Meanwhile, only 10% of adults and 16% of pediatric patients reported headaches while taking a placebo.
Compared to other Wegovy side effects, these percentages are fairly low. In the same trials, 44% of adults experienced nausea, 30% diarrhea, and 24% constipation — just to name a few.
Does the time of day you inject semaglutide affect whether it causes headaches?
It isn’t known at this time whether the time of day you inject semaglutide affects whether it causes headaches. But it is important to follow a consistent dosing regimen to minimize side effects on semaglutide. Specifically, it’s recommended that you take semaglutide on the same day of the week each week, but the time you take it that day is up to you.
Why do I feel so bad on semaglutide?
Semaglutide can cause a long list of side effects, ranging from nausea and vomiting to heartburn and hair loss. Semaglutide’s gastrointestinal side effects are more common during the initial dose escalation phase, but, thankfully, they usually lessen with time as your body gets used to the medication. If you’re continuing to experience severe or persistent side effects, talk to your healthcare provider. They may adjust your dosage or have you switch from semaglutide to another treatment option, such as tirzepatide.
How does semaglutide affect the brain?
Researchers are still learning about how semaglutide works. They already know that GLP-1 drugs like semaglutide act on brain receptors involved in appetite regulation. In addition to its positive effects on body weight, blood sugar control, and heart health, a growing body of research suggests it may even help lower the risk of cognitive decline and dementia. However, some people also report brain fog on Ozempic, although it’s possible that — like headaches — that could be linked to dehydration or low blood sugar.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Ozempic Important Safety Information: Read more about serious warnings and safety info.
Wegovy Important Safety Information: Read more about serious warnings and safety info.
GLP-1 Important Safety Information: Read more about serious warnings and safety info.
Saxenda Important Safety Information: Read more about serious warnings and safety info.
Mounjaro Important Safety Information: Read more about serious warnings and safety info.
Zepbound Important Safety Information: Read more about serious warnings and safety info.
References
Arca, K. N. & Singh, R. B. H. (2021). Dehydration and headache. Current Pain and Headache Reports, 25(8), 56. doi: 10.1007/s11916-021-00966-z. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8280611/
Baraness, L. & Baker, A. M. (2023). Acute Headache. I Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554510/
Canadian Agency for Drugs and Technologies in Health. (2019). Clinical Review Report: Semaglutide (Ozempic): (Novo Nordisk Canada Inc.): Indication: For the treatment of adult patients with type 2 diabetes mellitus to improve glycemic control, in combination with metformin (second-line treatment), and in combination with metformin and sulfonylurea (third-line treatment). Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK544016/
Gorgojo-Martínez, J. J., Mezquita-Raya, P., Carretero-Gómez, J., et al. (2022). Clinical Recommendations to Manage Gastrointestinal Adverse Events in Patients Treated with Glp-1 Receptor Agonists: A Multidisciplinary Expert Consensus. Journal of Clinical Medicine, 12(1), 145. doi: 10.3390/jcm12010145. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9821052/
Haghdoost, F. & Togha, M. (2022). Migraine management: non-pharmacological points for patients and health care professionals. Open Medicine, 17(1), 1869-1882. doi: 10.1515/med-2022-0598. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9691984/
Islam, M. R. & Nyholt, D. R. (2022). Glucose-related traits and risk of migraine - a potential mechanism and treatment consideration. Genes, 13(5), 730. doi: 10.3390/genes13050730. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9141901/
Khorsha, F., Mirzababaei, A., Togha, M., et al. (2020). Association of drinking water and migraine headache severity. Journal of Clinical Neuroscience: Official Journal of the Neurosurgical Society of Australasia, 77, 81–84. doi: 10.1016/j.jocn.2020.05.034. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32446809/
Kopp, K. O., Glotfelty, E. J., Li, Y., et al. (2022). Glucagon-like peptide-1 (GLP-1) receptor agonists and neuroinflammation: Implications for neurodegenerative disease treatment. Pharmacological Research, 186, 106550. doi: 10.1016/j.phrs.2022.106550. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9712272/
MedlinePlus. (2023). Headache. Retrieved from https://medlineplus.gov/ency/article/003024.htm
MedlinePlus. (2024). Low blood sugar. Retrieved from https://medlineplus.gov/ency/article/000386.htm
Nakhleh, A. & Shehadeh, N. (2021). Hypoglycemia in diabetes: An update on pathophysiology, treatment, and prevention. World Journal of Diabetes, 12(12), 2036–2049. doi: 10.4239/wjd.v12.i12.2036. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8696639/
Stovner, L. J., Hagen, K., Linde, M., & Steiner, T. J. (2022). The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. The Journal of Headache and Pain, 23, 34. doi: 10.1186/s10194-022-01402-2. Retrieved from https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-022-01402-2
U.S. Food & Drug Administration (FDA-a). (2025). Highlights of Prescribing Information: Ozempic (semaglutide) injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/209637s035,209637s037lbl.pdf
U.S. Food & Drug Administration (FDA-b). (2025). Highlights of Prescribing Information: Rybelsus (semaglutide) tablets, for oral use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/213051s024,s028s029lbl.pdf
U.S. Food & Drug Administration (FDA-c). (2025). Highlights of Prescribing Information: Wegovy (semaglutide) injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/215256s023lbl.pdf
U.S. Food & Drug Administration (FDA-d). (2025). Highlights of Prescribing Information: Zepbound (tirzepatide) injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/217806s031lbl.pdf
Wilding, J. P. H., Batterham, R. L., Calanna, S., et al. (2021). Once-weekly semaglutide in adults with overweight or obesity. New England Journal of Medicine, 384, 989-1002. doi: 10.1056/NEJMoa2032183. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa2032183