Key takeaways
In some clinical trials, people taking Ozempic lost around 11 pounds within the first 12 weeks, though results vary.
Common causes of slow weight loss on Ozempic include being early in treatment, low dosing, diet or exercise gaps, stress, poor sleep, and certain health conditions or medications.
Adjusting your diet, physical activity, stress levels, and sleep habits, along with speaking to your healthcare provider, can all help improve your weight loss results on Ozempic.
Here's what we'll cover
Key takeaways
In some clinical trials, people taking Ozempic lost around 11 pounds within the first 12 weeks, though results vary.
Common causes of slow weight loss on Ozempic include being early in treatment, low dosing, diet or exercise gaps, stress, poor sleep, and certain health conditions or medications.
Adjusting your diet, physical activity, stress levels, and sleep habits, along with speaking to your healthcare provider, can all help improve your weight loss results on Ozempic.
If you're not losing weight on Ozempic as expected, you're not alone. Studies show nearly 17% of people lose less than 5% of their body weight on semaglutide (the active ingredient in Ozempic). So, what’s the deal?
Below are 11 proven reasons why you might not be experiencing weight loss on Ozempic — plus specific solutions to get your progress back on track.
But first, what’s a typical weight loss timeline on Ozempic?
By three months, people usually lose around 11 pounds (and sometimes up to 15 pounds) on Ozempic.
With continued use, you can lose 15%–17% of your body weight in over a year or more. (Depending on your starting weight, this can equal 30+ pounds.)
1. You may need to be a bit more patient
If you’ve just started taking Ozempic, that may explain why you’re not seeing weight loss results.
It can take up to three (sometimes four) months to reach the full maintenance dosage of Ozempic. This is because the medication must be gradually increased over several weeks (i.e. titrated) to help reduce side effects and help your body adjust safely.
Be patient and rest assured that the medication is working, even if you’re not at your final dosage or losing weight just yet.
In studies, people taking 1 mg of Ozempic reported eating less, feeling less hungry, and having fewer cravings, particularly for high-fat foods, by around 12 weeks of treatment. As a result, many of the participants began to lose weight during this early period. But more noticeable changes typically occurred after reaching high or maintenance doses.
2. You may need a higher dosage of Ozempic
People taking higher doses of Ozempic tend to lose more weight. (They also tend to experience more intense side effects, for what it’s worth, though individual experiences may vary.)
After about a year on semaglutide, people who don’t have diabetes often lose around 15% of their body weight. People who also have type 2 diabetes usually lose less, about 7%–10% of their body weight.
Remember, those numbers are averages. Everybody reacts differently to medication, and the weight loss you experience on Ozempic may differ from someone else’s. Differences between individual experiences can also be due to differences in diet, activity levels, and other reasons we’ll get into below.
If you’re still on a lower dose of Ozempic (0.5 mg or 1 mg), you may want to talk with your healthcare provider about a dosage increase. Another option to ask about is Wegovy. This injectable medication contains the same active ingredient as Ozempic (semaglutide), but is available in higher doses that are approved specifically for weight loss.
3. You may need to make more changes to your diet
Ozempic is designed to be taken in combination with lifestyle changes like a reduced-calorie diet and increased physical activity. If you haven’t changed up your diet, now’s the time to do that and see how it affects your weight loss on Ozempic.
Here’s what to do:
Reduce your overall caloric intake by 500–750 calories daily while still staying in a safe range for your body.
Limit your consumption of starches, refined carbohydrates, sugar-sweetened beverages, alcohol, and red meat. (These are all associated with weight gain).
Practice mindful eating — i.e. eating without distractions and taking time to savor your food. Research shows this can lead to weight loss, especially when you are also adding exercise to your routine.
Talk to a healthcare provider or registered dietitian for more ideas on how to adjust your diet to improve weight loss on Ozempic.
4. You may need to eat more protein and fiber
If you’re not getting enough protein and fiber every day, it could be slowing your weight loss on Ozempic.
Protein and fiber help you feel full and satisfied for longer, which can naturally lead to eating less throughout the day. So eating foods high in these macronutrients can make weight loss on Ozempic more effective.
Good sources of protein include:
Meat
Fish
Poultry
Milk and other dairy products (e.g. Greek yogurt)
Soy-based foods (e.g. tofu, tempeh)
Beans and other legumes (e.g. lentils)
Nuts and nut butters
Quinoa
How much protein should you eat on Ozempic? For most adults, the recommended protein intake is about 0.8 grams per kilogram of body weight per day (or roughly about 10%--35% of daily calories).
When trying to lose weight, aiming higher — around 1.2–1.6 grams per kilogram per day — can help you feel fuller and protect muscle while you lose fat.
Fiber-rich foods include:
Fruits (with the peel; that’s where the fiber is)
Vegetables
Beans and other legumes
Nuts and seeds (in moderation, as these tend to be high calorie)
Whole grains (e.g. oat, barley)
How much fiber should you eat on Ozempic? Experts recommend 25 grams of fiber daily for women and 38 grams per day for men. After age 50, fiber needs are slightly lower so those recommendations come down to 21 grams daily for women and 30 grams daily for men.
Find your recommended protein intake
Calculate your recommended daily protein needs for weight loss, maintaining weight, or building muscle, based on your current weight and activity level.
Recommended protein intake
0 – 0
Grams/Day
0 – 0
Grams/Meal
This calculator provides general estimates and should not replace professional medical advice. Always consult a healthcare provider or registered dietitian before making significant changes to your diet or nutrition plan.
5. You may need to increase your physical activity
As mentioned above, Ozempic should be used in combination with a reduced-calorie diet and increased exercise.
While exercise on its own is limited in its ability to promote significant weight loss, it does help in combination with a reduced-calorie diet. Plus, it’s essential for keeping weight off on a long-term basis.
Here’s how exercise can support weight loss on Ozempic:
Start with 150 minutes of moderate-intensity exercise per week and gradually increase to 300 minutes per week. Think: Brisk walking, hiking, or riding a bike. (New to exercise? Start low, go slow, and be sure to clear any major changes to your exercise routine with your healthcare provider.)
Pair exercise with a lower-calorie diet. This one-two punch leads to more weight loss, according to research.
Combine aerobic with resistance training for an extra metabolism boost. Together, these workouts can help you build muscle mass while you lose fat, especially when you combine them with a high-protein diet.
6. You may need a different treatment
Ozempic gets a lot of attention, but it’s not the only option for weight loss — and it’s not even FDA-approved specifically for that use. It also isn’t always the most effective choice for everyone.
For example, Zepbound (tirzepatide), is an FDA-approved medication for weight loss. In less than a year and a half, people taking Zepbound lost between 15%–21% of their body weight depending on their dose — an average of 35–52 pounds.
In studies directly comparing Zepbound vs. Ozempic:
People taking Zepbound (tirzepatide) lost significantly more weight than those taking semaglutide.
Over about a year to a year and a half, this difference averaged roughly 15–20 pounds more weight loss with Zepbound compared with the highest-dose semaglutide
Think you may benefit from a different
Not losing weight on Ozempic and think you may benefit from switching meds? Talk with your healthcare provider. Other options — such as Zepbound, Wegovy, or Saxenda (liraglutide)— may be more effective for you.
7. You’re not taking Ozempic as prescribed
Do you sometimes forget to take Ozempic or skip doses altogether? If you’re not losing weight on Ozempic as quickly as you’d hoped to, you may want to stop doing that (unless you were expressly told to by your healthcare provider).
Like any prescription drug, it’s in your best interest to take Ozempic as prescribed. This ensures the medication works at its best.
The half-life of Ozempic lasts about one week — just in time for you to take your next dose. (Friendly reminder: The half-life is how long it takes for the amount of a drug in your body to reduce by half.)
Drug makers create dosing schedules based on a drug’s half-life in order to optimize a drug’s efficacy. So, if you regularly skip doses of Ozempic or get casual with your dosing regimen, the medication may not work as well as it’s supposed to — and you may not lose as much weight.
Here’s how to stay on track with your Ozempic dosing schedule:
Set reminders so you never miss a dose
Pair your dose with another activity you reliably do every week, like grocery shopping
When traveling, make a plan ahead of time so you can still take your dose as scheduled (or change the dosing day if needed).
It’s also important to follow any lifestyle changes your health provider recommends while taking Ozempic. These may include eating less, adjusting your diet, or getting more exercise.
8. You’ve reached a plateau
Those who have dieted before may be familiar with the unwelcome (though not uncommon) phenomenon of the dreaded weight loss plateau. If you’ve been taking Ozempic for a while and feel like your weight loss has slowed down, a plateau may be the culprit.
When people start dieting and exercising, it’s common to lose a lot of weight quickly in the beginning. But there may come a point when the weight loss slows down significantly.
This is known as the plateau, and it can happen when you lose too much muscle and fat simultaneously. As a result, your metabolism starts to slow — and so does your weight loss.
Hormonal changes can also occur during this period, so you might feel hungrier for high-calorie foods. Ozempic can help with these cravings, but in the meantime, don’t blame yourself.
A weight loss plateau is a normal part of losing weight for many people.
Here’s how you can break through a weight loss plateau on Ozempic:
Keep exercising, especially strength or resistance training, which helps build muscle. As you build muscle, your metabolism will catch up.
Watch for hidden calories, such as those in sugary drinks, juices, alcohol, or highly processed foods. Replace these items them with lower-calorie options when possible.
Increase protein intake, which helps you feel fuller and makes it easier to maintain a lower-calorie diet.
Move more throughout the day, not just during workouts. Research shows that simply walking more, sitting less, and even fidgeting all add up to more calories burned.
9. You may be too stressed out
If you’re not losing as much weight as you expected on Ozempic, it could be due to stress. Stress can lead to weight gain, whether it’s chronic stress from work or personal issues or a specific stressful event, like losing a loved one.
In addition to that, obesity itself can be a stressor due to the social stigma. And the more of these stressors you’re dealing with, the more weight you may gain.
Stress can contribute to weight gain in several ways:
It makes it harder to find time to make healthy meals.
It makes you less likely to exercise.
It makes you more likely to crave sugary, calorie-dense foods that slow down weight loss.
It affects your hormone levels, and parts of your brain and gut that impact how hungry you feel and what foods you crave.
It disrupts your sleep (more on this in the next section).
Try these stress management techniques to support weight loss on Ozempic:
Meditation or visualization
Yoga or tai chi
Deep breathing exercises
Progressive muscle relaxation
Therapy
10. You may not be sleeping well
Even your sleep habits may explain why you’re not losing weight on Ozempic. That’s because poor sleep habits — whether you’re sleeping too much or too little — are also linked to weight gain.
Here’s how:
People who get fewer than six hours or more than eight hours of sleep are more likely to gain weight in the long run.
People who sleep too little experience hormonal changes that impact their perception of hunger and crank up their cravings for foods high in calories and refined carbohydrates.
Sleeping too much (more than 10 hours daily) is also linked to obesity, as well as other health conditions that are connected to weight, such as diabetes and hypertension (high blood pressure).
If you’re not losing weight on Ozempic, try these tips for better sleep:
Aim for 7–9 hours of sleep per night
Establish a calming bedtime routine.
Avoid caffeine, alcohol, heavy meals, and electronics in the evening.
Go to bed and wake up at the same time every day — even weekends.
11. You may have other conditions like type 2 diabetes
Finally, other health conditions you’re managing can affect how quickly you lose weight on Ozempic.
If you have type 2 diabetes, which Ozempic is FDA-approved to treat, you will likely lose weight slower than those who are taking Ozempic solely to treat their obesity and who do not have type 2 diabetes.
Consider these results from one study:
After three months of taking semaglutide, people without type 2 diabetes lost 6.3% of their body weight, on average, compared with 3.9% for those with type 2 diabetes.
After six months, those without type 2 diabetes had lost 11.8%, while those with type 2 diabetes lost 7.2%.
Even the lower numbers still represent significant changes in body weight. But it’s helpful to remember that other conditions may make your weight loss a bit slower with Ozempic.
Not losing weight on Ozempic? You could even may also be taking certain medications that cause weight gain, thereby slowing your progress. Common culprits include antidepressants and steroid medications.
If you have other health conditions or are taking certain medications, ask your healthcare provider how they might affect your weight loss on Ozempic.
Your provider can help you adjust your weight loss expectations, if needed. They may also suggest an alternative drug if it’s a fit and your slowed weight loss (or weight gain) is really bothering you. (Do not make any changes to your treatment without first chatting with your provider.)
How to make Ozempic more effective
Taking Ozempic is one of many positive changes you can make toward a healthier lifestyle. Follow these healthy habits to make Ozempic more effective.
Change what you eat and how you eat
The key to losing weight, whether or not you’re taking Ozempic, is eating fewer calories than you burn.
Start by reducing your daily calorie intake by ~500 calories. Many people aim for around 1,500 calories per day or less. But the right target depends on your body, activity level, and your healthcare provider’s recommendations.
Consider adopting a Mediterranean or vegetarian diet, both of which have been proven to help with weight loss and better blood sugar control. One study found that following a Mediterranean diet for one year led to a weight loss of nearly 9%.
Limit or avoid salty, sugary, and fatty foods, as well as red meat and processed food.
Eat more vegetables, fruits, lean proteins, and whole grains. Even small changes, such as choosing healthier snacks or cutting out one type of high-calorie food or alcohol, can help with weight loss.
Limit late-night snacking and eating too late at night. Both of these habits can lead to weight gain and negatively impact your sleep cycle.
Eat smaller portions and try to slow down while eating, really focusing on savoring your food.
Move more
People taking Ozempic may want to start with 150 minutes of exercise per week. But exercising for longer can lead to more weight loss and maintenance. Experts generally recommend at least 200 minutes of physical activity per week to prevent weight gain and maintain weight loss while on Ozempic.
Ultimately though, start with whatever amount of exercise you can stick with. Even short workout sessions can help prevent additional weight gain. Plus, they can make it easier for you to develop a habit that grows into more exercise and more significant weight loss.
Other tips to ensure you move more:
Schedule workouts in your calendar.
Listen to music or a podcast to make it more fun.
Get up every hour and walk around your house or office for a few minutes.
Most importantly, find a workout routine that you enjoy. Resistance training is important for building muscle mass and keeping your metabolism working. But aerobic, resistance, and flexibility exercises can all offer benefits, too.
Remember to start low and go slow with exercise, especially if you have other medical conditions. Speak with your healthcare provider to make sure you are cleared for exercise before making any drastic changes in your routine.
Choose healthy habits
In addition to diet and exercise, explore other healthy habits you can develop to support your weight loss journey on Ozempic.
Limit alcohol and cut out smoking.
Find a stress management technique that gives you relief, whether it’s yoga, deep breathing exercises, meditation, or a mix of the above.
Sleep for 7–9 hours per night.
Stay hydrated. Drinking more water can help relieve many of Ozempic’s gastrointestinal side effects and could even help with weight loss.
Seek support from family and friends. Research shows this can make you more likely to lose weight on Ozempic.
Find an accountability partner. In a 15-week study, people who chose a weight loss “buddy” lost more weight than those who didn’t. And those who found buddies who really cheered each other on experienced the greatest reductions in their body mass index (BMI) and waist size.
Talk to your healthcare provider
Finally, talk to your healthcare provider and ask them why you’re not losing weight on Ozempic.
There may be other weight loss strategies that are more tailored to your body and your health situation. They may also want to try switching you to an alternative weight loss medication like Wegovy, Saxenda, or Zepbound.
The TL;DR? Don’t despair if you’re not losing as much weight as you expected on Ozempic. Try out a few of the strategies above, and see if they make a difference. In the meantime, try to enjoy the process, be patient, and talk to a health professional about what else they recommend you do.
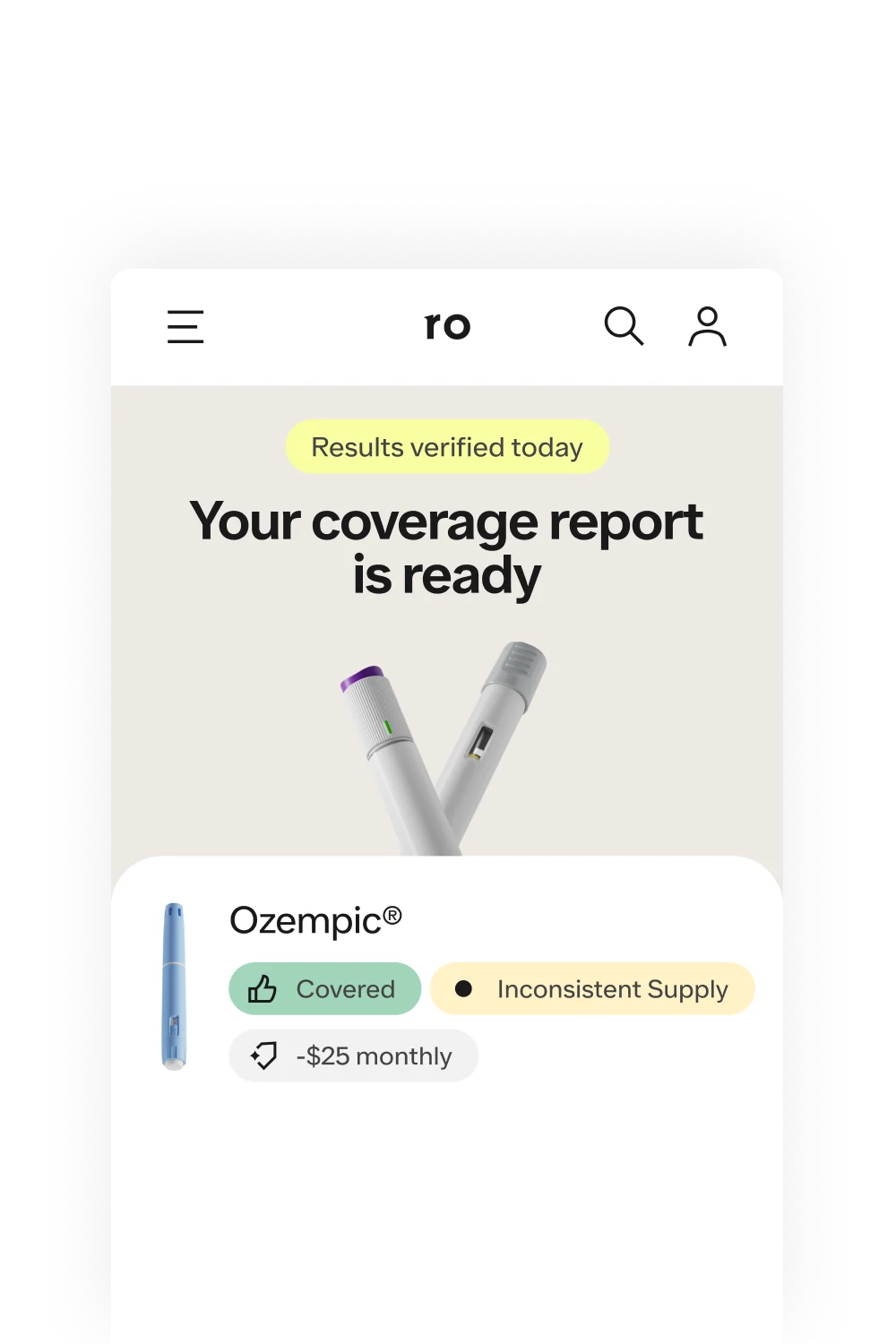
Rx weight loss with Ro
Get access to prescription weight loss medication online
Bottom line
Sometimes, it takes longer than you expect to lose weight on Ozempic. But the good news is that there’s usually a reason why. Here’s what to keep in mind:
You might simply need more time. It usually takes 3–4 months to reach your full dosage of Ozempic.
You might need a higher dosage, or a different medication altogether. People tend to lose more weight on higher doses of Ozempic or on medications approved specifically for weight loss, like Wegovy or Zepbound.
You may need to make more changes to your diet. Cutting calories, eating fewer processed foods, and eating more protein and fiber can make a noticeable difference.
You might need to up your exercise routine. Aim for at least 150–300 minutes per week and include resistance training to boost muscle mass and avoid weight loss plateaus.
You might need more sleep or less stress. These lifestyle factors can affect weight loss, too.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Ozempic Important Safety Information: Read more about serious warnings and safety info.
Wegovy Important Safety Information: Read more about serious warnings and safety info.
Zepbound Important Safety Information: Read more about serious warnings and safety info.
Saxenda Important Safety Information: Read more about serious warnings and safety info.
References
Akbar, A. & Shreenath, A. P. (2023). High Fiber Diet. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559033/
Aronne, L. J., Horn, D. B., le Roux, C. W., et al. (2025). Tirzepatide as Compared with Semaglutide for the Treatment of Obesity. New England Journal of Medicine, 393(1), 26-36. doi: 10.1056/NEJMoa2416394. Retrieved from https://pubmed.ncbi.nlm.nih.gov/40353578/
Blundell, J., Finlayson, G., Axelsen, M., et al. (2017). Effects of once-weekly semaglutide on appetite, energy intake, control of eating, food preference and body weight in subjects with obesity. Diabetes, Obesity & Metabolism, 19(9), 1242–1251. doi: 10.1111/dom.12932. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5573908/
Cox, C. E. (2017). Role of Physical Activity for Weight Loss and Weight Maintenance. Diabetes Spectrum: A Publication of the American Diabetes Association, 30(3), 157–160. doi: 10.2337/ds17-0013. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5556592/
Dailey, R., Romo, L., Myer, S., et al. (2018). The Buddy Benefit: Increasing the Effectiveness of an Employee-Targeted Weight-Loss Program. Journal of Health Communication, 23(3), 272–280. https://doi.org/10.1080/10810730.2018.1436622. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29452062/
Davies, M., Færch, L., Jeppesen, O. K., et al. (2021). Semaglutide 2.4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): a randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. Lancet, 397(10278), 971–984. doi: 10.1016/S0140-6736(21)00213-0. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33667417/
Hallare, J. & Gerriets, V. (2025). Half Life. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554498/
Harding, J. L., Backholer, K., Williams, E. D., et al. (2014). Psychosocial stress is positively associated with body mass index gain over 5 years: evidence from the longitudinal AusDiab study. Obesity (Silver Spring, Md.), 22(1), 277–286. doi: 10.1002/oby.20423. Retrieved from https://onlinelibrary.wiley.com/doi/10.1002/oby.20423
Hills, A. P., Byrne, N. M., Lindstrom, R., et al. (2013). 'Small changes' to diet and physical activity behaviors for weight management. Obesity Facts, 6(3), 228–238. doi: 10.1159/000345030. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5644785/
Jastreboff, A. M., Aronne, L. J., Ahmad, N. N., et al. (2022). Tirzepatide Once Weekly for the Treatment of Obesity. The New England Journal of Medicine, 387(3), 205–216. doi: 10.1056/NEJMoa2206038. Retrieved from https://www.nejm.org/doi/10.1056/NEJMoa2206038
Kim, J. Y. (2021). Optimal Diet Strategies for Weight Loss and Weight Loss Maintenance. Journal of Obesity & Metabolic Syndrome, 30(1), 20–31. doi: 10.7570/jomes20065. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8017325/
Léger, D., Beck, F., Richard, J. B., et al. (2014). The risks of sleeping "too much". Survey of a National Representative Sample of 24671 adults (INPES health barometer). PloS One, 9(9), e106950. doi: 10.1371/journal.pone.0106950. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4165901/
Leidy, H. J., Clifton, P. M., Astrup, A., et al. (2015). The role of protein in weight loss and maintenance. The American Journal of Clinical Nutrition, 101(6), 1320S–1329S. doi: 10.3945/ajcn.114.084038. Retrieved from https://www.sciencedirect.com/science/article/pii/S0002916523274274
Mason, A. E., Epel, E. S., Aschbacher, K., et al. (2016). Reduced reward-driven eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: Data from the SHINE randomized controlled trial. Appetite, 100, 86–93. doi: 10.1016/j.appet.2016.02.009. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4799744/
MedlinePlus. (2023). Protein in diet. Retrieved Feb. 20, 2024 from https://medlineplus.gov/ency/article/002467.htm
Mettler, S., Mitchell, N., & Tipton, K. D. (2010). Increased protein intake reduces lean body mass loss during weight loss in athletes. Medicine and Science in Sports and Exercise, 42(2), 326–337. doi: 10.1249/MSS.0b013e3181b2ef8e. Retrieved from https://journals.lww.com/acsm-msse/fulltext/2010/02000/increased_protein_intake_reduces_lean_body_mass.14.aspx
Mozaffarian, D., Hao, T., Rimm, E. B., et al. (2011). Changes in diet and lifestyle and long-term weight gain in women and men. The New England Journal of Medicine, 364(25), 2392–2404. doi: 10.1056/NEJMoa1014296. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3151731/
Novo Nordisk. (2025). Ozempic® Side Effects | Ozempic® (semaglutide) injection 0.5 mg or 1 mg. Retrieved from https://www.ozempic.com/how-to-take/side-effects.html
Ojeniran, M., Dube, B., Paige, A., et al. (2021). Semaglutide for weight loss. Canadian Family Physician, 67(11), 842. doi: 10.46747/cfp.6711842. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8589135/
Papamichou, D., Panagiotakos, D. B., & Itsiopoulos, C. (2019). Dietary patterns and management of type 2 diabetes: A systematic review of randomised clinical trials. Nutrition, Metabolism, and Cardiovascular Diseases, 29(6), 531–543. doi: 10.1016/j.numecd.2019.02.004. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30952576/
Parmar, R. M. & Can, A. S. (2023). Dietary Approaches to Obesity Treatment. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK574576/
Sarwan, G. & Rehman, A. (2024). Management of Weight Loss Plateau. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK576400/
Strasser, B. (2013). Physical activity in obesity and metabolic syndrome. Annals of the New York Academy of Sciences, 1281(1), 141–159. doi: 10.1111/j.1749-6632.2012.06785.x. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3715111/
Swift, D. L., Johannsen, N. M., Lavie, C. J., et al. (2014). The role of exercise and physical activity in weight loss and maintenance. Progress in Cardiovascular Diseases, 56(4), 441–447. doi: 10.1016/j.pcad.2013.09.012. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3925973/
Thornton, S. N. (2016). Increased Hydration Can Be Associated with Weight Loss. Frontiers in Nutrition, 3, 18. doi: 10.3389/fnut.2016.00018. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4901052/
Tomiyama, A. J. (2019). Stress and Obesity. Annual Review of Psychology, 70, 703–718. doi: 10.1146/annurev-psych-010418-102936. Retrieved from https://www.annualreviews.org/content/journals/10.1146/annurev-psych-010418-102936
Tzoulis, P. & Baldeweg, S. E. (2024). Semaglutide for weight loss: unanswered questions. Frontiers in Endocrinology, 15, 1382814. doi: 10.3389/fendo.2024.1382814. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11188346/
U.S. Food and Drug Administration (FDA-a). (2025). Highlights of Prescribing Information: Ozempic (semaglutide) injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/209637s035,209637s037lbl.pdf
U.S. Food & Drug Administration (FDA-b). (2025). Highlights of Prescribing Information: Zepbound (tirzepatide) Injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/217806s031lbl.pdf
Vadher, K., Patel, H., Mody, R., et al. (2022). Efficacy of tirzepatide 5, 10 and 15 mg versus semaglutide 2 mg in patients with type 2 diabetes: An adjusted indirect treatment comparison. Diabetes, Obesity & Metabolism, 24(9), 1861–1868. doi: 10.1111/dom.14775. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9546430/
von Loeffelholz, C. & Birkenfeld, A. L. (2022). Non-Exercise Activity Thermogenesis in Human Energy Homeostasis. Endotext. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK279077/
Wang, M. L., Pbert, L., & Lemon, S. C. (2014). Influence of family, friend and coworker social support and social undermining on weight gain prevention among adults. Obesity (Silver Spring, Md.), 22(9), 1973–1980. doi: 10.1002/oby.20814. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4435839/
Wilding, J. P. H., Batterham, R. L., Calanna, S., et al. (2021). Once-Weekly Semaglutide in Adults with Overweight or Obesity. The New England Journal of Medicine, 384(11), 989–1002. doi: 10.1056/NEJMoa2032183. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa2032183