Key takeaways
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist that mimics your natural gut-produced GLP-1 hormone.
While it’s not indicated for weight loss, some healthcare providers may prescribe it off-label for that purpose.
In the first six weeks of taking Ozempic, you may notice some weight loss, though results will vary depending on factors unique to you.
Small and sustainable lifestyle changes to diet, exercise, sleep, and stress may help maximize your results with Ozempic.
Here's what we'll cover
Key takeaways
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist that mimics your natural gut-produced GLP-1 hormone.
While it’s not indicated for weight loss, some healthcare providers may prescribe it off-label for that purpose.
In the first six weeks of taking Ozempic, you may notice some weight loss, though results will vary depending on factors unique to you.
Small and sustainable lifestyle changes to diet, exercise, sleep, and stress may help maximize your results with Ozempic.
Whether you are considering taking Ozempic (semaglutide) or have just been prescribed this medication for weight loss, you may understandably have oodles of questions, including “When does Ozempic start working?” and “How fast can you lose weight on Ozempic?”
The answer is, it depends. Ozempic starts working right away, but that doesn’t necessarily mean you’ll lose weight immediately. Your individual experience and results might be influenced by factors like your dosage, starting weight, underlying conditions, and more.
However, experts agree that pairing Ozempic with healthy lifestyle changes can help optimize your weight loss results in both the short and long term.
In this article, we’ve outlined what to expect in your first six weeks of taking Ozempic for weight loss. Plus, we’ll share tips to help maximize your results and maintain momentum and motivation throughout treatment.
Getting started with Ozempic: what to know
Ozempic is a type of medication called a glucagon-like peptide-1 (GLP-1) receptor agonist. These medications work by copycatting the GLP-1 incretin hormone that your body produces naturally. Your intestines release this hormone when you eat.
The US Food and Drug Administration (FDA) first approved Ozempic in 2017 to treat type 2 diabetes, but some healthcare providers may also prescribe Ozempic off-label for weight loss to help treat obesity, a chronic condition.
How Ozempic works
GLP-1 has several roles, including increasing insulin secretion, reducing appetite, and slowing digestion. Ozempic works by binding to and activating these GLP-1 receptors. This activation can help regulate blood sugar and may also promote weight loss through various mechanisms, including:
Slowing gastric emptying, which can help you feel fuller longer
Decreasing hunger cues in the brain, which can help quiet “food noise,” a nonmedical term for an intrusive preoccupation with food
Improving insulin sensitivity and helping with better blood sugar control, which may also aid weight loss
Weight loss timeline
Weight loss on Ozempic can take time. The amount of weight you can lose in the first few weeks on Ozempic will depend on various factors, such as your starting weight, other health conditions, and more.
Your healthcare provider will likely start you on the lowest dose to see how well you tolerate Ozempic. From there, they may gradually increase your dose every four weeks until you reach a maintenance dose.
Also, because Ozempic is not indicated for weight management, research on its effectiveness solely for weight loss is limited. Most clinical trials reporting weight loss outcomes involved people taking 2.4 mg of semaglutide, the maximum dose of Wegovy (a version of semaglutide that’s specifically indicated for weight loss). The maximum dose of Ozempic is 2 mg of semaglutide.
Still, existing research can offer some clues as to how effective semaglutide is for weight loss overall.
In the first few weeks, you might notice some weight loss, but your body may need time to adjust to the medication before you see more dramatic results. In the primary study evaluating semaglutide for weight loss, participants, on average, lost about 2% of their body weight in the first four weeks of treatment.
A 2022 cohort study analyzed weight loss outcomes in 175 people with obesity or overweight who were taking 1.7 mg or 2.4 mg of semaglutide for six months. The results showed that, on average, participants lost about 6% of their body weight at three months (about 12 weeks) and 11% at six months (about 24 weeks).
When combined with diet and exercise changes, Ozempic may lead to more significant weight loss over the long term. In the same primary study on semaglutide, participants lost 15% of their body weight in a little over a year (68 weeks).
The 6-week weight loss plan with Ozempic
Just as everyone’s weight loss journey is different, your personal experience with Ozempic treatment will be unique. Remember: GLP-1 medications like Ozempic are not meant to be quick fixes. These are long-term medications that are designed to be used with a balanced diet and regular exercise for optimal results.
Here’s a general idea of what you might expect in your first several weeks on Ozempic, along with some tips for managing common side effects and maximizing your treatment.
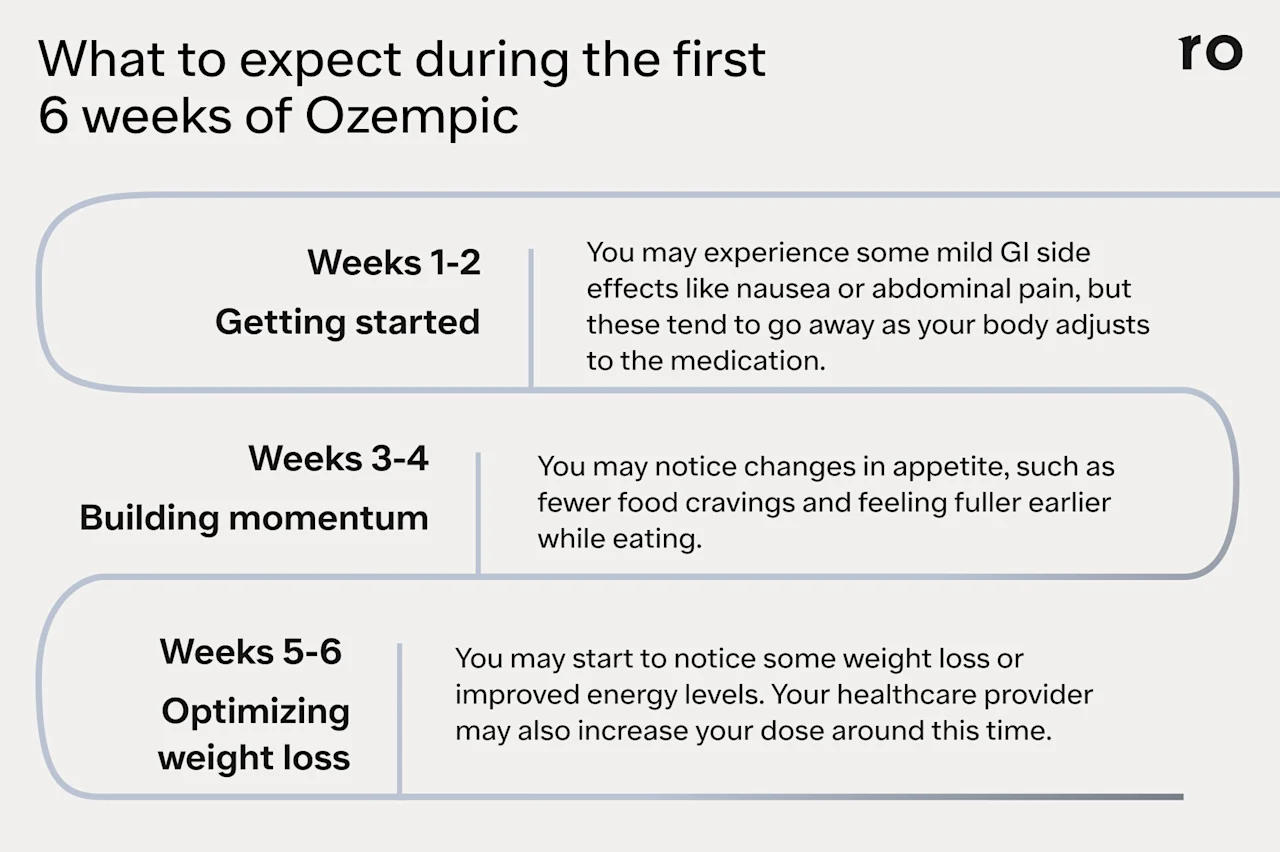
Week 1–2: starting Ozempic
Ozempic comes in a pre-filled pen that you inject under the skin (in the thigh, abdomen, or upper arm) once weekly, on the same day and time each week.
The medication comes in four dose strengths: 0.25 mg, 0.5 mg, 1 mg, and 2 mg. Your healthcare provider may administer your first dose in the office to show you where and how to inject Ozempic at home.
Ozempic has gone through extensive testing and is considered safe, but it may cause some gastrointestinal (GI) discomfort when you’re first getting started or when you change dose strengths.
Your healthcare provider will likely start you on the lowest dose (0.25 mg) to help your body gradually adjust to the medication and help minimize side effects.
The most common side effects of Ozempic may include:
Abdominal pain
Constipation
Diarrhea
Nausea
Vomiting
These GI side effects tend to be mild, and they may go away as your body adjusts to the medication. If you experience any side effects, talk to your healthcare provider right away so they can help you address any discomfort.
Tips for minimizing Ozempic side effects
Stay hydrated with regular sips of water to help food move through your GI tract and minimize any unpleasant side effects. Drinking plenty of water can also help prevent dehydration if you experience diarrhea or vomiting.
Eat smaller, more frequent meals and avoid heavy, fried, or rich foods to help minimize nausea. You may also want to ask your healthcare provider about anti-nausea medication.
Add more high-fiber foods to your diet or take a fiber supplement (such as psyllium husk) if you experience constipation.
This is also a great time to start incorporating more physical activity into your routine.
If you’re new to exercise or haven’t been active for a while, try gentle exercises, such as walking or yoga, to get started.
Go slow and build on your progress over time—even a little more movement throughout the day can add up!
Week 3–4: building momentum
You may notice appetite changes, such as feeling fuller earlier while eating, staying satisfied for longer, and having fewer cravings.
If you haven’t already, now is the time to incorporate healthy dietary changes to complement your reduced appetite on Ozempic.
Tips for building momentum
Start with small, sustainable diet changes, like eating more fruits and vegetables or swapping out sweetened drinks for water or herbal tea.
Set aside time each week for meal planning. If you have a variety of nutritious meals and snacks on hand, you might be less likely to reach for convenience foods that are high in sodium, sugar, or processed carbohydrates when you’re on the go. Plus, research suggests that meal prepping is associated with a healthier diet that may support weight loss.
Slowly start to increase the intensity or duration of your workouts. For example, bump your usual 20-minute walk up to 30 minutes, or add a few jogging intervals into your trek.
Week: 5–6: optimizing weight loss
Your healthcare provider may move you to the next dose increment (usually 0.5 mg) around week five. However, for various reasons unique to you, they may keep you at the initial starting dose for longer.
Now that you’ve been on Ozempic for about a month and have begun incorporating sustainable lifestyle changes, you may start to notice some weight loss, but the number on the scale may not be the only change you see.
Some people who take Ozempic report boosted confidence, having more energy, and feeling more motivated to try new hobbies and activities. Pay attention to how you feel and any other positive changes you experience in the first few weeks. These are all wins worth celebrating!
In these weeks, consider focusing your efforts on building consistency, which can help you reach your goals as you continue to take Ozempic.
Tips for building consistency
Keep building on your fitness practice. For example, if you’ve been working out two days per week, try adding a third. It might also be a good time to incorporate strength training into your routine.
Schedule exercise on your calendar as you would any other commitment in your life. Some research shows that exercising at the same time each day can help you maintain consistency.
Remember to focus on progress rather than perfection. If you miss a day of scheduled exercise, which may happen due to illness or a scheduling snafu, just try again the next day.
What happens after 6 weeks?
Check in with your healthcare provider around the six-week mark to evaluate your progress so far. If you’re tolerating the medication well and seeing gradual improvements in weight loss, they may decide to keep you at your current dose.
If you’re not losing weight, your healthcare provider may prescribe a higher dose around week eight. The goal is to find the lowest dose that allows you to see results while minimizing side effects.
Keep in mind that Ozempic is designed as a long-term treatment. In most clinical trials, people saw the most significant weight loss after a year or longer on semaglutide. Your healthcare provider may recommend staying on Ozempic even after you reach your target weight goal. If you stop taking Ozempic too soon, you might regain some or most of the weight you lost.
You should continue to follow up with your healthcare provider every few weeks so they can monitor your progress, help mitigate side effects, and address any questions or concerns you might have.
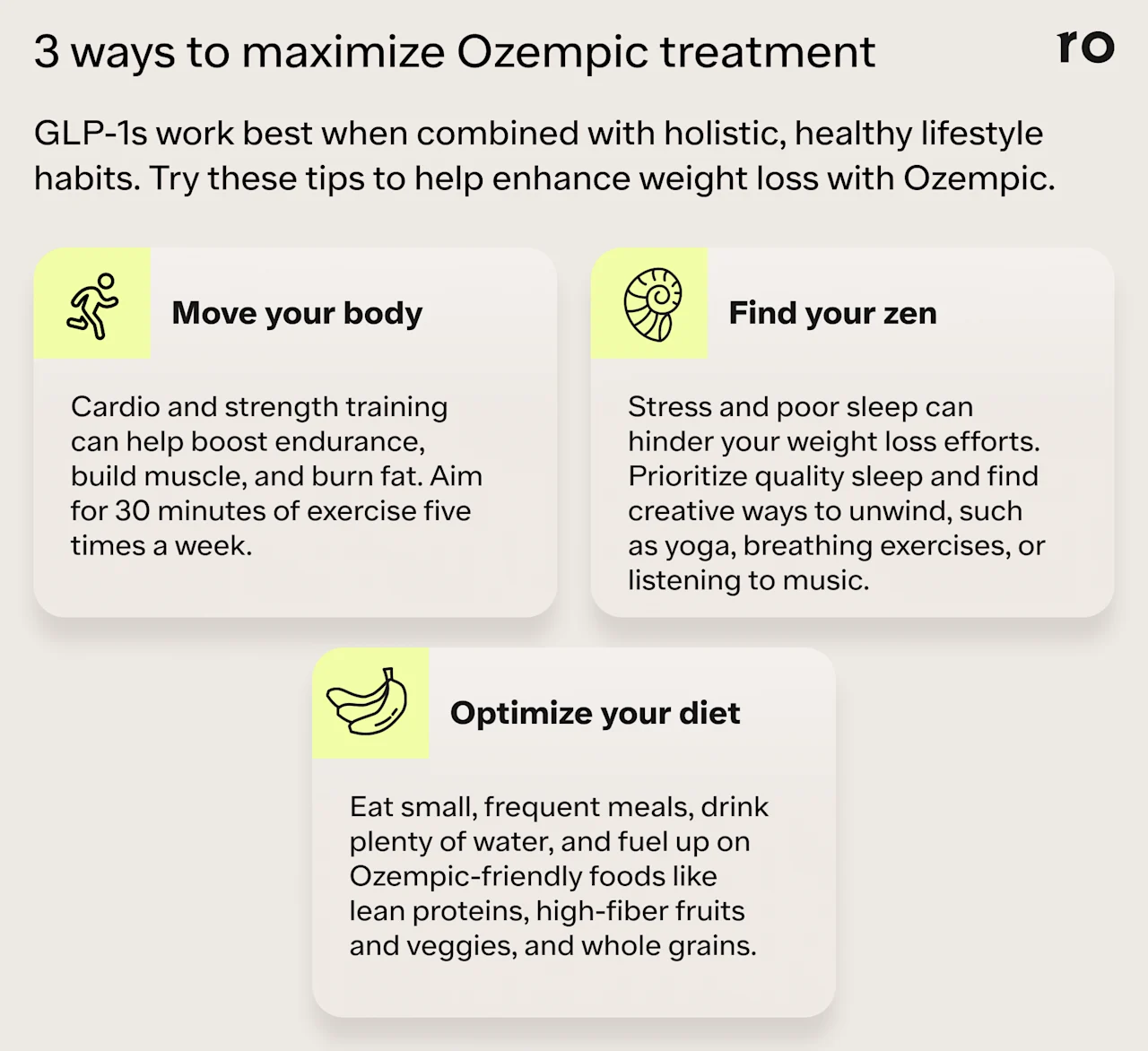
Tips to maximize weight loss with Ozempic
Ozempic works best in conjunction with sustainable diet and lifestyle changes. Regular exercise, a balanced diet, and better sleep and stress management can help support your weight loss treatment and set the foundation for better health overall. They may also help prevent weight gain if you decide to stop taking Ozempic.
You don’t have to make a ton of changes all at once, which can lead to burnout or make it harder to stick to these habits in the long term. Instead, gradually incorporate these tips into your daily routine, maybe by starting with one or two new changes and adding one subsequent change each week over your first six weeks.
Diet changes
Reduce or eliminate ultra-processed foods. Foods like crackers, processed meat, and soft drinks are generally high in sodium, unhealthy fats, and added sugar. These ingredients can contribute to insulin resistance and the accumulation of visceral fat. They can also drive cravings for more ultra-processed foods, which are designed to be highly palatable and possibly even addictive.
Eat more fruits and vegetables. These high-fiber foods feed the gut microbiome, creating short-chain fatty acids, which then help produce more natural GLP-1 hormone. They are also packed with antioxidants that can help lower inflammation and improve overall health. Fiber has the added benefit of helping you feel fuller from meals and snacks. Fruit is also a great substitute when you’re craving something sweet.
Include more protein in your diet. Protein can help you feel more satisfied and can help slow the absorption of glucose into the bloodstream. This, in turn, can help promote insulin sensitivity, which can aid with weight loss. Protein also supports muscle. Muscle mass can help increase insulin sensitivity and may boost the number of calories you burn at rest.
Exercise recommendations
Incorporate strength training into your workouts. Increasing muscle mass can boost the amount of calories you burn at rest and improve insulin sensitivity. Strength training is also particularly important for people on Ozempic, as some of the weight you lose may include some muscle. Aim for at least two strength training sessions per week.
Up your cardio. Aerobic exercise can get your heart rate up and help improve your endurance. Choose activities you enjoy—if exercise is boring or feels like a chore, you’re less likely to stick with it. Although dedicated exercise sessions help, you can also build mini cardio sessions into your day by taking the stairs, walking briskly on your commute, or dancing around your kitchen after dinner.
Lifestyle adjustments
Get at least 7-9 hours of quality sleep per night. Poor sleep can make you more insulin-resistant the next day and may lead to cravings. Sleep can also help regulate cortisol, the “stress hormone.” Although we need cortisol to function, too much of this hormone can contribute to weight gain.
Find creative ways to relieve stress. Chronic stress can increase cortisol, which may lead to weight gain. Techniques such as meditation, yoga, and spending time with loved ones can help keep your stress levels in check.
Common challenges and how to overcome them
Weight loss is an ongoing journey rather than something that changes quickly and remains permanent. For this reason, several challenges can crop up, from side effects and weight loss plateaus to feeling a lack of motivation at times.
Here are a few tips to help overcome these challenges if they arise.
Managing side effects
If you experience side effects, be sure to talk to your healthcare provider. Some side effects will go away with time, but that doesn’t mean you have to suffer if you’re uncomfortable. Your provider may reduce your dose or offer other solutions to help mitigate side effects that are bothersome to you.
Breaking through weight loss plateaus
Research on semaglutide suggests that your weight loss progress may continue for more than 60 weeks (a little over a year). Your body may stop shedding weight for various reasons, including reaching a weight that’s healthy for your frame, height, and body composition.
If your weight loss stalls before you’ve reached your goal weight, talk to your provider. They may increase your dose (if you’re not already taking the maximum dose), or they might suggest other diet, exercise, and lifestyle changes to help support your progress.
Staying motivated
Motivation can wax and wane for anyone—even the most driven athletes. Understanding the difference between motivation and discipline can help. Motivation is your internal drive to take action to achieve a goal. Discipline is the ability to consistently take action even when motivation falters.
For example, you may find that on some days you just don’t feel like exercising. Skipping a day here and there when you’re sick, extra tired, or have a packed schedule will not derail your progress. Instead, it can even offer you a reset.
Having discipline means that you’ll get back to exercise the next day (or close to it) and that you’ll again maintain consistency as much as possible. But discipline is not about being perfect; it’s about building a habit that you engage in most of the time.
Other things that might help boost motivation include journaling to track your progress, asking a friend or loved one to be your exercise partner, or joining a weight loss support group to find encouragement and connect with others taking GLP-1s.
Bottom line
Ozempic starts working as soon as you take it, but it may take a while before you experience weight loss. The first six weeks are a great time to make small and sustainable lifestyle changes to help complement Ozempic’s mechanisms of action and produce the best results long term.
Some research suggests that you could lose around 2-4% of your body weight in the first six weeks on Ozempic, but your results will vary depending on factors like dosage, starting weight, overall health, and others.
In the first six weeks, focus on small changes to help build the foundation for healthy habits. That might include going for a walk every day, eating more fruits and veggies, or drinking more water.
You may experience some mild GI side effects when you first start taking Ozempic. Your healthcare provider can help you find ways to minimize discomfort while your body adjusts to the medication.
Ozempic can be an effective tool for weight loss, but it’s not a silver bullet or quick fix. It’s a long-term medication that people may take for a year or longer to see and maintain weight loss results. Lifestyle factors like a balanced diet and regular exercise also play an important role in weight loss results with Ozempic.
Talk to your healthcare provider if you have any questions or concerns, such as increased side effects or stalled weight loss. They can evaluate your treatment and make adjustments as needed.
Frequently asked questions (FAQs)
How much weight can I lose in 6 weeks with Ozempic?
Weight loss results on Ozempic are highly individual and depend on factors like starting weight, time on the medication, health status, and more. However, some clinical trial data suggests that people on Ozempic might realistically expect to lose less than 3% of their body weight in the first six weeks.
How long does it take to lose 20 pounds on Ozempic?
How long it takes to lose 20 pounds on Ozempic varies from person to person. In clinical trials, on average people who take semaglutide can lose about 6% of their body weight in three months, 11% in six months, and 15% in 1.25 years.
How much weight can you lose in a month on Ozempic?
Ozempic starts working right away, but the amount of weight you can lose in a month will depend on individualized factors such as your dosage, starting weight, and overall health. In one double-blind trial studying semaglutide for obesity, participants lost an average of 2% of their body weight after about four weeks on the medication.
How to speed up weight loss on Ozempic?
Ozempic is not a quick-fix medication. Losing weight on Ozempic is a gradual process. However, incorporating lifestyle changes can help optimize your results. In most clinical trials studying semaglutide for weight loss, participants paired medication with a reduced-calorie diet and about 150 minutes of exercise each week.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Ozempic Important Safety Information: Read more about serious warnings and safety info.
GLP-1 Important Safety Information: Read more about serious warnings and safety info.
Wegovy Important Safety Information: Read more about serious warnings and safety info.
References
Collins, L. & Costello, R. A.. (2024). Glucagon-Like Peptide-1 Receptor Agonists. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK551568/
Ducrot, P., Méjean, C., Aroumougame, V., et al. (2017). Meal planning is associated with food variety, diet quality and body weight status in a large sample of French adults. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 12. doi: 10.1186/s12966-017-0461-7. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28153017/
Dugardin, C., Fleury, L., Touche, V., et al. (2022). An exploratory study of the role of dietary proteins in the regulation of intestinal glucose absorption. Frontiers in Nutrition, 8, 769773. doi: 10.3389/fnut.2021.769773. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8808719/
Gearhardt, A. N. & DiFeliceantonio, A. G. (2023). Highly processed foods can be considered addictive substances based on established scientific criteria. Addiction, 118(4), 589-598. doi: 10.1111/add.16065. Retrieved from https://pubmed.ncbi.nlm.nih.gov/36349900/
Ghusn, W., De la Rosa, A., Sacoto, D., et al. (2022). Weight loss outcomes associated with semaglutide treatment for patients with overweight or obesity. JAMA Network Open, 5(9), e2231982. doi: 10.1001/jamanetworkopen.2022.31982. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9486455/
Jensterle, M., Ferjan, S., Ležaič, L., et al. (2023). Semaglutide delays 4-hour gastric emptying in women with polycystic ovary syndrome and obesity. Diabetes, Obesity, and Metabolism, 25(4), 975-984. doi: 10.1111/dom.14944. Retrieved from https://pubmed.ncbi.nlm.nih.gov/36511825/
Kohanmoo, A., Faghih, S., & Akhlaghi, M. (2020). Effect of short- and long-term protein consumption on appetite and appetite-regulating gastrointestinal hormones, a systematic review and meta-analysis of randomized controlled trials. Physiology and Behavior, 226, 113123. doi: 10.1016/j.physbeh.2020.113123. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32768415
Ma, J., Sloan, M., Fox, C. S., et al. (2014). Sugar-sweetened beverage consumption is associated with abdominal fat partitioning in healthy adults. The Journal of Nutrition, 144(8), 1283. doi: 10.3945/jn.113.188599. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4093984/
Müller, T. D., Finan, B., Bloom, S. R., et al. (2019) Glucagon-like peptide 1 (GLP-1). Molecular Metabolism, 30, 72-130. doi: 10.2174/1573399816666200705210006. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32628589/
Nunes, E. A., Colenso-Semple, L., McKellar, S. R., et al. (2022). Systematic review and meta-analysis of protein intake to support muscle mass and function in healthy adults. Journal of Cachexia, Sarcopenia, and Muscle, 13(2), 795-810. doi: 10.1002/jcsm.12922. Retrieved from https://pubmed.ncbi.nlm.nih.gov/35187864/
Schumacher, L. M., Thomas, J. G., Raynor, H. A., et al. (2019). Relationship of consistency in timing of exercise performance and exercise levels among successful weight loss maintainers. Obesity (Silver Spring), 27(8), 1285-1291. doi: 10.1002/oby.22535. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31267674/
van Eekelen, E., Geelen, A., Alssema, M., et al. (2019). Sweet snacks are positively and fruits and vegetables are negatively associated with visceral or liver fat content in middle-aged men and women. Journal of Nutrition, 149(2), 304-313. doi: 10.1093/jn/nxy260, Retrieved from https://pubmed.ncbi.nlm.nih.gov/30657914/
Vinelli, V., Biscotti, P., Martini, D., et al. (2022). Effects of dietary fibers on short-chain fatty acids and gut microbiota composition in healthy adults: a systematic review. Nutrients, 14(13), 2559. doi: 10.3390/nu14132559. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9268559/
Wender, C. L. A., Manninen, M., & O’Connor, P. J. (2022). The effect of chronic exercise on energy and fatigue states: a systematic review and meta-analysis of randomized trials. Frontiers in Psychology, 13, 907637. doi: 10.3389/fpsyg.2022.907637. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9206544/
Wilding, J. P. H., Batterham, R. L., Calanna, S., et al. (2021). Once-weekly semaglutide in adults with overweight or obesity. New England Journal of Medicine, 384(11), 989-1002. doi: 10.1056/NEJMoa2032183. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa2032183